Anticholinergic Burden Calculator
Add Medications
Your Anticholinergic Burden
Combining tricyclic antidepressants (TCAs) like amitriptyline with common over-the-counter antihistamines like diphenhydramine (Benadryl) might seem harmless-especially if you're trying to manage pain and sleep at the same time. But this combo is one of the most dangerous, yet overlooked, drug interactions in modern medicine. It doesn’t just cause drowsiness or dry mouth. It can trigger confusion, urinary retention, rapid heartbeat, hallucinations, and even permanent cognitive damage. And it’s happening more than you think.
What Is Anticholinergic Overload?
Your body uses acetylcholine, a key neurotransmitter, to control muscle movement, heart rate, digestion, memory, and alertness. Anticholinergic drugs block this chemical. A single anticholinergic medication might cause mild side effects. But when you stack two or more-like a TCA and a first-generation antihistamine-you overload the system. This is called anticholinergic burden or overload.It’s not just about feeling groggy. High anticholinergic load can shut down parts of your brain responsible for memory and decision-making. A 2015 JAMA Internal Medicine study found people who took high-burden anticholinergics for just three years had a 54% higher risk of developing dementia. And it’s not just older adults. Anyone taking these drugs long-term is at risk.
Why TCAs and Antihistamines Are a Perfect Storm
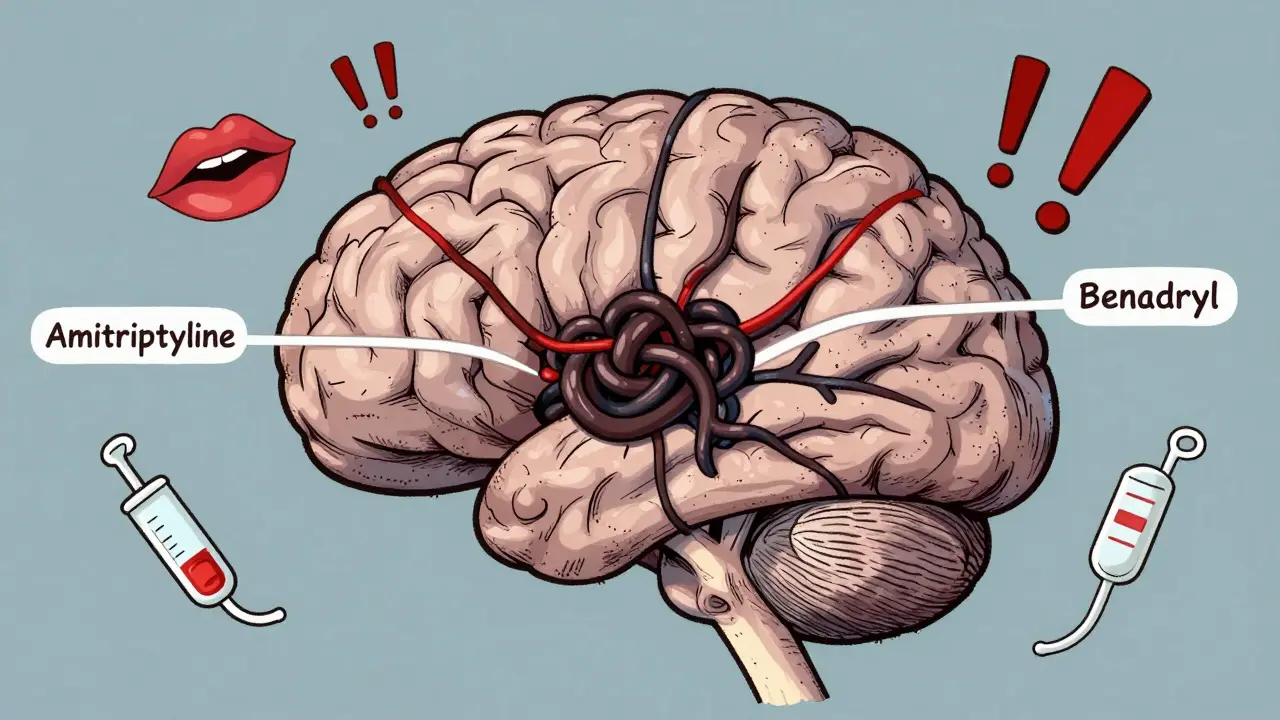
Tricyclic antidepressants were developed in the 1950s. Drugs like amitriptyline, imipramine, and clomipramine work by increasing serotonin and norepinephrine in the brain. But they also strongly block muscarinic acetylcholine receptors. Amitriptyline, for example, has a Ki value of 8.9 nM at the M1 receptor-meaning it binds tightly and stays active for hours.First-generation antihistamines like diphenhydramine and hydroxyzine were designed to block histamine to reduce allergies. But they also block acetylcholine receptors. Diphenhydramine’s Ki is higher (1,000 nM), but people take it in doses of 25-50 mg-much higher than typical TCA doses. When combined, their effects multiply.
It’s not additive. It’s exponential. The Anticholinergic Cognitive Burden (ACB) scale rates amitriptyline as a 3 (highest risk) and diphenhydramine as a 2. Together, that’s a score of 5. Research shows a score of 4 or higher doubles the risk of dementia. And this isn’t theoretical. A 2020 Elsevier study tracked 3,365 patients and found over 6,800 high-risk alerts for TCA-antihistamine combinations.
Who’s Most at Risk?
Older adults are the most vulnerable. Their livers and kidneys don’t clear drugs as efficiently. Their brains have fewer acetylcholine receptors to begin with. But the problem isn’t limited to seniors. People with chronic pain, depression, or insomnia often get prescribed TCAs and then reach for Benadryl to help sleep. That’s a red flag.One patient on Psych Forums described being rushed to the ER after her doctor added Benadryl to her amitriptyline regimen. She developed urinary retention and severe confusion. Her diagnosis? Anticholinergic toxicity.
Medical residents report seeing this regularly. A Reddit user on r/medschool shared that three elderly patients they encountered in the hospital had delirium traced directly to TCA-antihistamine combinations prescribed by primary care doctors who didn’t realize the cumulative effect.
It’s Not Just Benadryl
Many people don’t realize how many OTC products contain diphenhydramine. It’s in sleep aids like Tylenol PM, Unisom, and Sominex. It’s in cold and flu formulas like NyQuil and Dimetapp. Even some allergy pills like Benadryl Allergy Plus Congestion have it.Hydroxyzine (Atarax, Vistaril) is another common offender. Prescribed for anxiety or itching, it’s just as potent as diphenhydramine when it comes to blocking acetylcholine. And it’s often paired with TCAs in pain clinics.
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are different. They barely touch acetylcholine receptors. Their ACB score is 0. If you need an antihistamine, these are the only safe options if you’re on a TCA.
What About Other Antidepressants?
Not all antidepressants carry this risk. SSRIs like sertraline (Zoloft) and fluoxetine (Prozac) have minimal anticholinergic activity. SNRIs like duloxetine (Cymbalta) and venlafaxine (Effexor) are also safer. Even among TCAs, some are less dangerous. Nortriptyline and desipramine have lower anticholinergic effects than amitriptyline or clomipramine.But here’s the catch: TCAs are still used because they work well for neuropathic pain, fibromyalgia, and treatment-resistant depression. So the goal isn’t to avoid them entirely-it’s to avoid stacking them with other anticholinergics.
A 2022 study in the Journal of Clinical Psychiatry found that 78% of psychiatrists now routinely check anticholinergic burden using the ACB scale-up from just 32% in 2018. That’s progress. But primary care doctors, who prescribe most of these combinations, aren’t always trained to do it.

How to Stay Safe
If you’re on a TCA, here’s what you need to do:- Check every medication you take. Look at the active ingredients in every pill, liquid, or patch. If it says “diphenhydramine,” “hydroxyzine,” or “doxylamine,” stop using it.
- Switch to non-anticholinergic sleep aids. Melatonin (0.5-5 mg) works for sleep without touching acetylcholine. Trazodone (low dose) is sometimes used off-label and has lower anticholinergic risk than TCAs or Benadryl.
- Ask for an ACB score. Ask your doctor or pharmacist to calculate your total anticholinergic burden. If it’s 4 or higher, you’re in danger zone.
- Monitor your cognition. If you notice memory lapses, trouble focusing, or confusion, speak up. Use the Mini-Mental State Examination (MMSE) as a rough check-scores below 24 suggest possible anticholinergic delirium.
- Don’t assume OTC means safe. Over-the-counter doesn’t mean low-risk. It means no prescription needed. That’s it.
What’s Changing in 2026?
The FDA now requires updated labeling on all TCAs and first-generation antihistamines to warn about cumulative anticholinergic effects. Electronic health records like Epic now block prescriptions that combine these drugs-92% of attempted co-prescriptions trigger hard stops.The American Geriatrics Society launched the Anticholinergic Burden Audit in 2023. Early results show 41% of inappropriate TCA-antihistamine pairs have been discontinued in participating clinics.
And a $2.4 million NIH study (2023-2026) is tracking long-term cognitive effects. Preliminary data shows that even 30 days of high-burden combinations increases delirium risk by 200% in people over 65.
Pharmacogenomic testing is also becoming more common. Some people have a CYP2D6 gene variant that makes them slow metabolizers. If you’re one of them and take a TCA with another CNS drug, your risk of toxicity jumps 3.2 times.
Bottom Line
You don’t need to stop your TCA if it’s working. But you absolutely need to stop any OTC antihistamine you’re taking with it. There’s no safe dose of diphenhydramine if you’re on amitriptyline. No exceptions.Anticholinergic overload doesn’t happen overnight. It builds silently-like a slow leak in a pipe. One pill here, one capsule there. Before you know it, your brain is drowning in blocked signals.
If you’re managing chronic pain or depression, you deserve relief. But you also deserve to keep your mind sharp. The safest path isn’t adding more drugs. It’s removing the ones that silently harm you.
Can I take Benadryl with amitriptyline?
No. Combining Benadryl (diphenhydramine) with amitriptyline creates a high-risk anticholinergic overload. Both drugs block acetylcholine, and together they can cause confusion, urinary retention, rapid heartbeat, hallucinations, and increase dementia risk. Even one dose can be dangerous in older adults. Switch to non-anticholinergic alternatives like loratadine or melatonin.
What are the signs of anticholinergic toxicity?
Symptoms include dry mouth, blurred vision, constipation, urinary retention, rapid heartbeat, confusion, memory problems, hallucinations, agitation, and delirium. In severe cases, it can lead to seizures, coma, or death. If you’re on a TCA and start feeling unusually foggy or have trouble urinating, seek medical help immediately.
Are all antihistamines dangerous with TCAs?
No. Only first-generation antihistamines like diphenhydramine, hydroxyzine, and doxylamine have strong anticholinergic effects. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) have little to no effect on acetylcholine and are safe to use with TCAs.
Is there a safer antidepressant than amitriptyline?
Yes. SSRIs like sertraline or escitalopram and SNRIs like duloxetine have much lower anticholinergic risk. Among TCAs, nortriptyline and desipramine are less anticholinergic than amitriptyline or clomipramine. But TCAs are still used for neuropathic pain because they work better for some people. The key is avoiding other anticholinergics, not necessarily switching antidepressants.
How do I know if I’m at risk for anticholinergic overload?
Check your total Anticholinergic Cognitive Burden (ACB) score. Amitriptyline = 3, diphenhydramine = 2, hydroxyzine = 2. Add up all your medications. If the total is 4 or higher, you’re at high risk. Older adults, people with kidney or liver issues, and those taking more than three anticholinergic drugs are especially vulnerable. Ask your pharmacist to calculate your score.
Can anticholinergic damage be reversed?
In many cases, yes. Stopping the offending drugs can lead to significant improvement in cognition within weeks to months. A 2023 study in the Journal of the American Geriatrics Society showed that deprescribing anticholinergics reduced cognitive decline by 34% over 18 months. The earlier you stop, the better your chances of recovery.



Comments
bro i took benadryl with amitriptyline for a week cause i couldnt sleep and woke up feeling like my brain was wrapped in saran wrap. no joke. couldnt remember my own phone number. went to the er and the doc looked at me like i just stole his lunch. turns out i was at acb score of 5. now i use melatonin and my mind feels like it came back from vacation. dont be me.
Wow. So you’re telling me OTC meds aren’t free passes to brain rot? Shocking.
Actually, I think this whole anticholinergic burden narrative is being wildly overblown by pharmaceutical interests trying to push SSRIs-because, let’s be honest, they make more money off them. I’ve been on amitriptyline for twelve years, took diphenhydramine for insomnia since 2015, and I’m sharper than most 30-year-olds. My memory? Excellent. My cognitive tests? Above average. The JAMA study? Small sample size, retrospective bias, and they didn’t control for sleep quality, which is the real culprit here. Also, I’m 67, and I’ve never had a hallucination-unless you count my dreams about being chased by a sentient toaster.
And don’t get me started on the FDA’s new labeling requirements-next they’ll mandate warning labels on water because hydration can cause water intoxication. This is fearmongering dressed up as science. People are scared of their own prescriptions now. They should be scared of the over-medicalization of normal human experiences. Sleep trouble? Take a warm bath. Chronic pain? Try yoga. But no-let’s just add another pill, then ban the one that helped you sleep, and call it progress.
Also, the ACB scale? A crude, arbitrary tool invented by pharmacists who’ve never held a human hand. It reduces complex neurochemistry to a math problem. My grandmother took three anticholinergics for decades and lived to 94, knitting sweaters and remembering every birthday. So forgive me if I don’t panic every time I see “diphenhydramine” on a label. I’ll take my chances with a little brain fog over the side effects of five different SSRIs that made me feel like a zombie with a credit card.
And yes, I know the 2020 Elsevier study. But correlation isn’t causation. Maybe people who take these meds are also more likely to be sedentary, eat processed food, or watch Netflix for 12 hours a day. Maybe the real cause is loneliness. Or bad coffee. Or the fact that we’re all just slowly rotting in this digital hellscape. But no, let’s blame the medicine. Always the medicine.
Also, trazodone? It’s a sedating SSRI with a half-life longer than my last relationship. I’d rather have the dry mouth than the emotional numbness. And don’t even get me started on melatonin-some people need 20mg to sleep, others get nightmares from 0.5mg. It’s not magic. It’s biology. And biology is messy. So stop pretending there’s a clean, safe, algorithmic solution to human suffering.
Finally, I’ve read the NIH study. It says “increased delirium risk by 200% in people over 65.” That’s a scary number. But what’s the baseline? 1%? 2%? Even if it doubles, that’s still 2-4%. That’s less than the risk of falling in your own bathroom. Should we ban bathtubs too?
I’m not saying this is harmless. But I’m saying: don’t let fear replace critical thinking. And if you’re going to write a post like this, at least acknowledge that some people benefit-and that not every elderly person is a walking dementia statistic.
I’m a nurse and I see this every week. A 72-year-old comes in confused, can’t urinate, heart racing. Family says they just added Benadryl for allergies. Doctor didn’t know the patient was on amitriptyline. Happens all the time. This isn’t theoretical. It’s real. Please, if you’re on a TCA, check every pill. Even the ones you’ve had for years.
sooo… you’re telling me the same doc who prescribed me 50mg of amitriptyline for fibro didn’t think to ask if i was takin’ nyquil for my cold? classic. i mean, i thought nyquil was just ‘sleep juice’ like my grandma used to say. turns out it’s basically liquid brain fog with a cherry flavor. now i’m on zyrtec and melatonin and i swear my thoughts aren’t moving through molasses anymore. also-why is everyone still using unisom? it’s literally just diphenhydramine in a fancy box. #pharmaisawasteofmoney
India has same problem-many doctors still prescribe cetirizine with amitriptyline, thinking it’s safe, but some patients report dizziness, memory lapse. Actually, many OTC brands in India contain diphenhydramine under different names like ‘Diphen’ or ‘Sedapin’. Even ‘sleep tablets’ sold at local pharmacies. Patients don’t read labels. And doctors? They’re overworked. I’ve seen 80-year-old women on 3 anticholinergics-no one checked. We need awareness posters in pharmacies. Not just in US. Here too.
I took amitriptyline for 5 years and diphenhydramine for 3. I lost 2 years of my life to fog. I forgot my daughter’s birthday. I cried for no reason. I thought I was going crazy. Then I stopped everything. Took 11 months to feel like myself again. Now I’m scared to even take Advil PM. I don’t trust medicine anymore. I don’t trust doctors. I don’t trust myself.
so i just checked my medicine cabinet and found 3 things with diphenhydramine. whoops. guess i’m not as chill as i thought. also i thought ‘PM’ meant ‘pretty magical’ not ‘profoundly messing with your brain’. thanks for the reality check. melatonin it is.
ACB score of 5? That’s wild. I’ve been using nortriptyline + loratadine for years and my pharmacist just ran my med list and said I’m at 1.5. So low risk. But I had no idea how much higher amitriptyline was. I’m switching. Also-did you know that some compounding pharmacies now make custom sleep formulas without anticholinergics? Like melatonin + magnesium + glycine. No diphenhydramine. No trazodone. Just… calm. I’m ordering some. Let me know if you want the recipe.
Oh wow, so the solution to modern medicine’s failures is… reading labels? Groundbreaking. Next you’ll tell us not to drink bleach. I mean, really? This is the hot take? The fact that people don’t know what’s in their meds is a national disgrace. But guess what? It’s not the drugs’ fault-it’s the system’s. Pharma markets these combos like candy. Doctors don’t have time to explain. Patients don’t read the tiny print. And now we’re all just walking time bombs with a CVS loyalty card. Congrats. You just diagnosed America.
How dare you suggest that Americans are too lazy to read labels? We’re the most informed, educated, and vigilant population on earth. This is a socialist plot to make us dependent on big pharma’s new ‘safe’ antidepressants. The real danger is losing our freedom to choose our own brain fog. 🇺🇸🔥
WHY IS NO ONE TALKING ABOUT HOW THE FDA IS SILENTLY ERASING OUR CHOICES?! 🤬 I used to take Benadryl because it made me feel like I was floating on a cloud of cotton candy. Now they’re gonna block it? That’s not safety-that’s tyranny. 🌈💊 #FreeMyDiphenhydramine #AnticholinergicLiberationFront
thanks for this. i was on amitriptyline and nyquil for months. never thought it was a problem. now i switched to zyrtec and melatonin. sleeping better, thinking clearer. no more brain fog. just wish i knew this 2 years ago.
You’re not alone. So many people are silently struggling with this. Thank you for sharing this vital information. Your post could save someone’s mind. Keep speaking up. Your voice matters. 💪🌿