What Is Polypharmacy-and Why Should You Care?
When someone over 65 is taking five or more medications at the same time, that’s called polypharmacy. It’s not always wrong-many older adults need multiple drugs to manage heart disease, diabetes, arthritis, or depression. But the more pills you take, the higher the risk of dangerous side effects, confusion, falls, and hospital stays. In the U.S., nearly half of adults over 65 are on five or more prescriptions. In nursing homes, it’s as high as 80%. And that number keeps climbing.
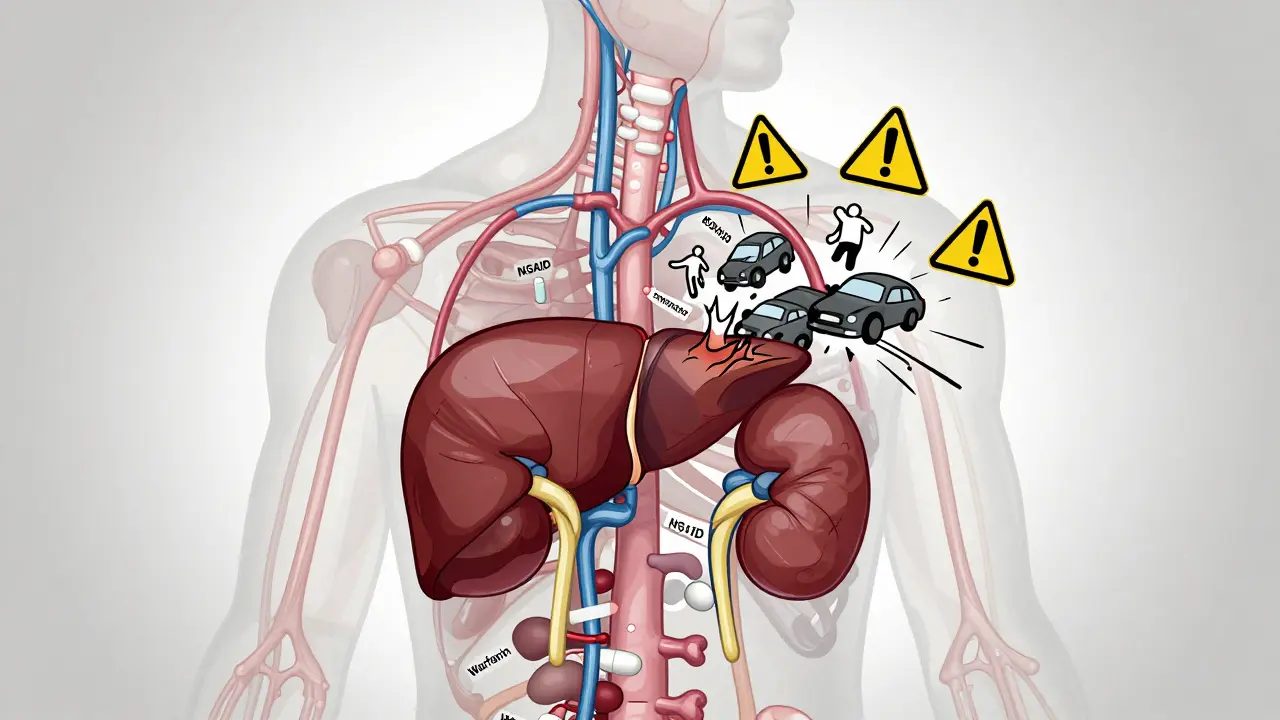
It’s not just about the quantity. It’s about what’s in those pills. A 78-year-old with high blood pressure might be on a beta-blocker. Add a painkiller like ibuprofen, and suddenly their kidneys are under strain. Throw in a sleeping pill and an antidepressant, and now their balance is off. One drug masks the side effect of another. That’s called a prescribing cascade-and it’s happening more than you think.
Why Older Bodies Handle Medicines Differently
Your body changes as you age. Your liver and kidneys don’t filter drugs the way they used to. That means medications stick around longer. A drug that was safe at 50 might become toxic at 75. Older adults also become more sensitive to certain medicines. Benzodiazepines, for example-used for anxiety or sleep-can cause dizziness, memory lapses, and falls. Yet they’re still prescribed too often.
Even over-the-counter drugs and supplements add up. A daily fish oil capsule, a turmeric tablet, or a melatonin gummy might seem harmless. But when combined with blood thinners or antidepressants, they can cause serious reactions. Studies show that nearly 40% of older adults don’t tell their doctor about their supplements. That’s a blind spot in safety.
The Hidden Dangers: Drug Interactions and Real Risks
With two medications, there’s a 6% chance of a bad interaction. With five, it jumps to 50%. With seven or more? The risk hits 100%. That’s not a guess-it’s based on clinical data from thousands of patients.
Common dangerous combos include:
- NSAIDs (like ibuprofen) + blood pressure meds → kidney damage
- Anticholinergics (used for overactive bladder or allergies) + antidepressants → confusion, memory loss
- Benzodiazepines + opioids → slowed breathing, higher death risk
- Warfarin + certain antibiotics or herbal supplements → bleeding
One study found that patients on ten or more drugs were over twice as likely to be hospitalized for a drug-related problem. And the biggest culprit? Pain medications. Nearly half of older adults on multiple prescriptions were taking NSAIDs or opioids-often without a clear plan to taper them.
Deprescribing: It’s Not Stopping Medicines. It’s Stopping the Right Ones.
Deprescribing isn’t about cutting pills just because there are too many. It’s about reviewing each one: Is this still helping? Is it doing more harm than good?
Think of it like decluttering your closet. You don’t throw everything out. You keep what fits, what’s useful, and what still serves you. The same goes for meds. The American Geriatrics Society’s Beers Criteria and the STOPP/START tools are used by doctors to spot medications that should be reconsidered in older adults. Examples:
- Long-term benzodiazepines for insomnia
- Proton pump inhibitors (PPIs) used for years without review
- Antipsychotics for dementia-related agitation
- Statins in very elderly patients with limited life expectancy
Stopping these doesn’t mean worsening disease. In fact, studies show that carefully planned deprescribing reduces falls by up to 22%, cuts emergency room visits, and improves quality of life. One trial found that older adults who had their sleep meds reduced reported better daytime alertness and fewer nighttime accidents.
Why Is Deprescribing So Hard?
If it’s so beneficial, why isn’t it happening more?
Doctors are stretched thin. A 15-minute appointment isn’t enough to review 12 medications. Many providers don’t feel trained in deprescribing. Others fear backlash-if a patient’s blood pressure rises after stopping a pill, they’ll blame the doctor, even if the drug was causing more harm than good.
Patients are scared, too. They’ve been told for years that these pills are life-saving. Asking to stop one feels like giving up. Some think, “If my doctor prescribed it, it must be necessary.” Others worry symptoms will come back worse.
And then there’s the system. In the U.S. and U.K., doctors are paid per visit, not per outcome. There’s no incentive to spend 45 minutes reviewing meds. Pharmacies don’t always share data between chains. Specialists prescribe without knowing what other doctors have ordered. It’s a broken chain.

What Can You Do? A Simple Action Plan
You don’t need to wait for your doctor to bring it up. Here’s how to take control:
- Make a full list-include every prescription, OTC drug, vitamin, herb, and supplement. Write down why you take each one. If you don’t know, write “Don’t know.”
- Bring it to your next appointment-ask: “Which of these are still necessary? Are any of these causing side effects I haven’t mentioned?”
- Ask about deprescribing-say: “Could we review my meds to see if anything can be safely reduced?”
- Use a pill organizer-but don’t rely on it alone. Make sure someone checks the list monthly.
- Involve your pharmacist-community pharmacists can spot dangerous combos you might miss. Many offer free med reviews.
One woman in Manchester, 82, was on 11 medications. She was dizzy, confused, and falling. Her GP didn’t know she was taking a herbal sleep aid. After a pharmacist-led review, three drugs were stopped-her sleep aid, a long-term PPI, and a low-dose antipsychotic. Within six weeks, her balance improved. Her memory cleared. She stopped going to the ER.
The Future: Better Tools, Better Care
Change is coming-slowly. Electronic health records now flag dangerous drug combos. Some clinics have pharmacists embedded in geriatric teams. AI tools are being tested to predict which patients are at highest risk for polypharmacy harm.
But the real shift needs to be cultural. Medication isn’t a trophy. More pills don’t mean better care. Sometimes, less is more. The goal isn’t to eliminate all meds-it’s to make sure every one has a reason to be there.
As the population ages, this won’t be optional. It’ll be essential. The question isn’t whether we’ll deprescribe. It’s whether we’ll do it before someone gets hurt.
Is polypharmacy always dangerous?
No-not always. Many older adults need multiple medications to manage chronic conditions like heart failure, diabetes, or arthritis. Polypharmacy becomes dangerous when medications are no longer needed, when they interact harmfully, or when side effects outweigh benefits. The key is regular review, not just the number of pills.
Can I stop my meds on my own if I think they’re causing problems?
Never stop a prescribed medication without talking to your doctor or pharmacist. Some drugs, like blood pressure pills or antidepressants, can cause dangerous withdrawal effects if stopped suddenly. Even if you feel fine, stopping abruptly can lead to rebound symptoms, increased heart rate, or seizures. Always ask for a safe tapering plan.
How often should older adults review their medications?
At least once a year-but ideally after every hospital visit, when a new doctor prescribes something, or if you notice new side effects like dizziness, confusion, fatigue, or falls. If you’re on five or more meds, ask for a formal medication review every six months.
What’s the difference between Beers Criteria and STOPP/START?
The Beers Criteria list specific drugs that older adults should avoid or use with caution. STOPP/START goes further: STOPP identifies potentially inappropriate prescriptions (like giving a sedative to someone with dementia), while START identifies drugs that are missing-like a statin for someone with heart disease who’s not on one. Together, they give a fuller picture of what’s wrong and what’s missing in a medication list.
Do pharmacists really help with deprescribing?
Yes. Community pharmacists have access to your full prescription history across pharmacies. They’re trained to spot interactions, duplicate therapies, and outdated prescriptions. Many offer free medication reviews. In the U.K., NHS pharmacists can work directly with GPs to adjust regimens-especially for older patients with complex needs.
Are herbal supplements safe to take with prescription drugs?
Not always. St. John’s Wort can reduce the effect of blood thinners and antidepressants. Garlic and ginkgo can increase bleeding risk. Turmeric may interfere with diabetes meds. Many older adults assume “natural” means safe-but supplements aren’t regulated like drugs. Always tell your doctor what you’re taking, even if it’s from the health food store.





Comments
This is the most irresponsible medical advice I've ever seen. You're telling people to just stop their meds? What if they die? Who's liable? My aunt took herself off blood pressure pills after reading some blog and ended up in the ER. This isn't 'decluttering'-it's medical negligence dressed up as wellness culture.
And don't even get me started on pharmacists. They're not doctors. They can't diagnose. They just hand out pills and collect paychecks. Let the professionals handle this, not some guy with a pill organizer and a YouTube playlist.
Ive been on 8 meds for 12 years and i feel fine so why change anything i mean if its not broke dont fix it right also my doc never asked me about my turmeric or fish oil so maybe they just dont care idk
So let me get this straight… the system is broken, doctors are lazy, and now we’re supposed to trust pharmacists who can’t even spell ‘pharmacy’ right on their signs?
Meanwhile, Big Pharma is laughing all the way to the bank while we’re over here Googling ‘can melatonin cause kidney stones’ at 3am.
Deprescribing sounds like a buzzword for ‘stop taking stuff because your insurance won’t cover it anymore.’
I love how this post calls it 'decluttering' like we're organizing a closet and not potentially yanking life-sustaining meds out from under someone.
But also… yikes. My grandma was on 14 pills. She didn’t even know what half of them were for. One day she stopped the blood thinner because she 'felt fine' and ended up with a stroke. So yeah, I get the intent. But this isn’t Marie Kondo. This is playing Russian roulette with your organs.
Also-why is no one talking about how the FDA approves drugs for 65-year-olds but the trials are done on 40-year-olds? We’re just guessing. All of it.
This is why America is falling apart. You want to take away pills? Fine. But first fix the healthcare system. Fix the nutrition. Fix the lack of exercise. Don’t just tell old people to stop their meds and call it 'empowerment.' We’re not in Sweden. We don’t have universal care. We have co-pays and surprise bills. Your 'simple action plan' means nothing when your doctor won’t see you for 3 months.
I’ve been a caregiver for my dad for 8 years. He was on 11 meds. We cut it down to 5 after a pharmacist review. He sleeps better. He doesn’t fall. He remembers my name.
It wasn’t easy. We cried. We were scared. But it worked.
Don’t let fear stop you from asking. Just don’t do it alone.
My uncle died after stopping his heart pill because some guy on Reddit said it was bad. Now his wife is alone. This is dangerous. Stop giving advice like you know everything. Not everyone has a smart phone or a PhD in medicine.
The 100% interaction rate with 7+ drugs is a lie. Source?
So… we’re supposed to trust doctors who got paid to prescribe, pharmacists who got paid to dispense, and then blame us when it all goes sideways? 😒
Meanwhile, my 80-year-old neighbor takes 12 pills, 3 supplements, and a CBD gummy that says 'for relaxation' on the label. She says she feels 'lighter.' I say she’s one missed dose away from a coma.
Less is more? Or just… less?
The data presented is compelling and aligns with peer-reviewed literature from the Journal of the American Geriatrics Society. However, implementation remains a systemic challenge. Deprescribing requires longitudinal care coordination, which is currently underfunded and underprioritized in most primary care models. A multidisciplinary approach-integrating clinical pharmacists, geriatricians, and care navigators-is not a luxury, it is a necessity.
I’ve worked in geriatrics for 22 years. The biggest myth? That patients don’t want to stop meds. They do. They’re just too scared to ask. I’ve had 78-year-olds cry because they thought their memory loss was 'just aging'-until we pulled the anticholinergic. Their eyes lit up. They remembered their granddaughter’s birthday.
It’s not about cutting pills. It’s about giving people back their lives. And yeah, it’s messy. But so is aging.
The assertion that polypharmacy is 'not always dangerous' is statistically misleading. The cumulative risk of adverse drug events increases exponentially with each additional medication, regardless of indication. Furthermore, the Beers Criteria are not universally adopted in clinical practice due to institutional inertia and lack of regulatory enforcement. The proposed action plan is insufficient without mandatory medication reconciliation protocols at every point of care transition.
My mother is 84. She takes 6 prescriptions. We didn’t know she was also taking ashwagandha from her yoga friend. When we told the pharmacist, he said, 'Oh, that’s why her INR was spiking.'
It’s not about trust. It’s about communication. And most of us just don’t know what to ask.
I’ve read this entire thing and I’m still not convinced. If you’re old enough to need 10 pills, you’re old enough to take them. This 'less is more' nonsense is just another trend from people who think yoga and kale fix everything. My dad’s on 14 meds and he’s still bowling every Wednesday. Don’t ruin his routine because you think you know better.
I’ve been on 8 meds for 15 years. I don’t sleep, I don’t eat, I don’t remember why I walked into the kitchen. But I take them. Because if I don’t, I’ll die. And I’m not ready. So don’t tell me to 'review' them. Tell the system to stop making me choose between my dignity and my life.