Branded combo pills often cost 10 to 50 times more than buying the same drugs as separate generics. Learn why this happens, who's paying the price, and how to save money without sacrificing care.
When you take a combination medication, a single pill that contains two or more active drugs designed to work together. Also known as fixed-dose combination, it’s not just convenience—it’s a strategy used to improve adherence, reduce pill burden, and sometimes boost effectiveness. Think of it like a team: one drug might lower blood pressure, while the other helps the first one work better or cuts down on side effects. This isn’t science fiction—it’s standard practice for conditions like high blood pressure, HIV, diabetes, and even depression.
But polypharmacy, the use of multiple medications at once. Also known as multiple drug therapy, it’s common in older adults and people with chronic conditions. And while combination pills help reduce the number of pills you swallow, they don’t eliminate the risks. Some combinations can cause unexpected drug interactions, when two or more medications affect each other’s absorption, metabolism, or effect in the body. Also known as medication interactions, they can lead to dizziness, kidney stress, or worse. That’s why knowing what’s in your combination pill matters. For example, some blood pressure combos include a diuretic and an ACE inhibitor—great for control, but dangerous if your kidneys are already weak. Or a diabetes combo with metformin and a DPP-4 inhibitor like saxagliptin: effective, but not for everyone.
Doctors use combination medications because they’re practical. But patients need to be just as informed. You can’t assume that because it’s one pill, it’s safer. The medication safety, the practice of using drugs in a way that minimizes harm and maximizes benefit. Also known as drug safety, it’s not just about avoiding side effects—it’s about asking the right questions: Why this combo? Are there alternatives? What happens if I stop one part? Many people don’t realize that if one drug in the combo causes a problem, you might have to switch the whole pill—even if the other drug is working fine. That’s why the posts here cover real cases: from how gabapentinoids stack up in combo regimens, to why some patients on SGLT2 inhibitors need to watch for ketoacidosis even when their sugar levels look normal. You’ll find guides on how to talk to your doctor about your meds, how to spot hidden risks in your prescription, and how pharmacists help optimize these regimens through Medication Therapy Management.
Whether you’re managing high blood pressure with a combo pill, treating HIV with a fixed-dose regimen, or just trying to simplify your daily routine, understanding combination medication means taking control—not just swallowing pills. The posts below give you the facts you need to ask better questions, spot red flags, and work smarter with your care team.
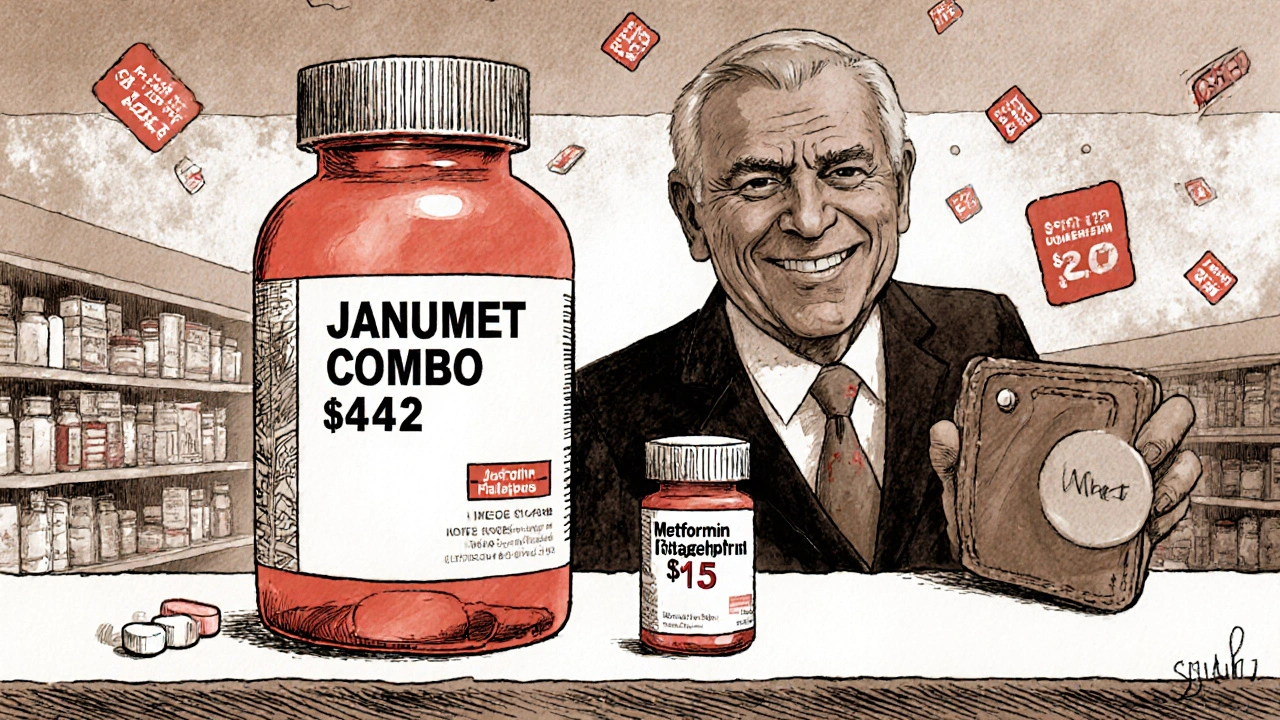
Branded combo pills often cost 10 to 50 times more than buying the same drugs as separate generics. Learn why this happens, who's paying the price, and how to save money without sacrificing care.