When you’re managing a chronic condition like high blood pressure or type 2 diabetes, taking multiple pills every day can be a hassle. That’s why doctors often prescribe combo generics-single pills that combine two or more drugs into one. But here’s the question most people don’t ask: Is that convenience worth the extra cost?
Turns out, it often isn’t. In 2016, Medicare Part D spent $925 million more on branded combination drugs than it would have if patients had simply bought the same active ingredients as separate generic pills. That’s not a rounding error. That’s enough money to cover free prescriptions for millions of seniors for a year.
Why Combo Drugs Cost So Much
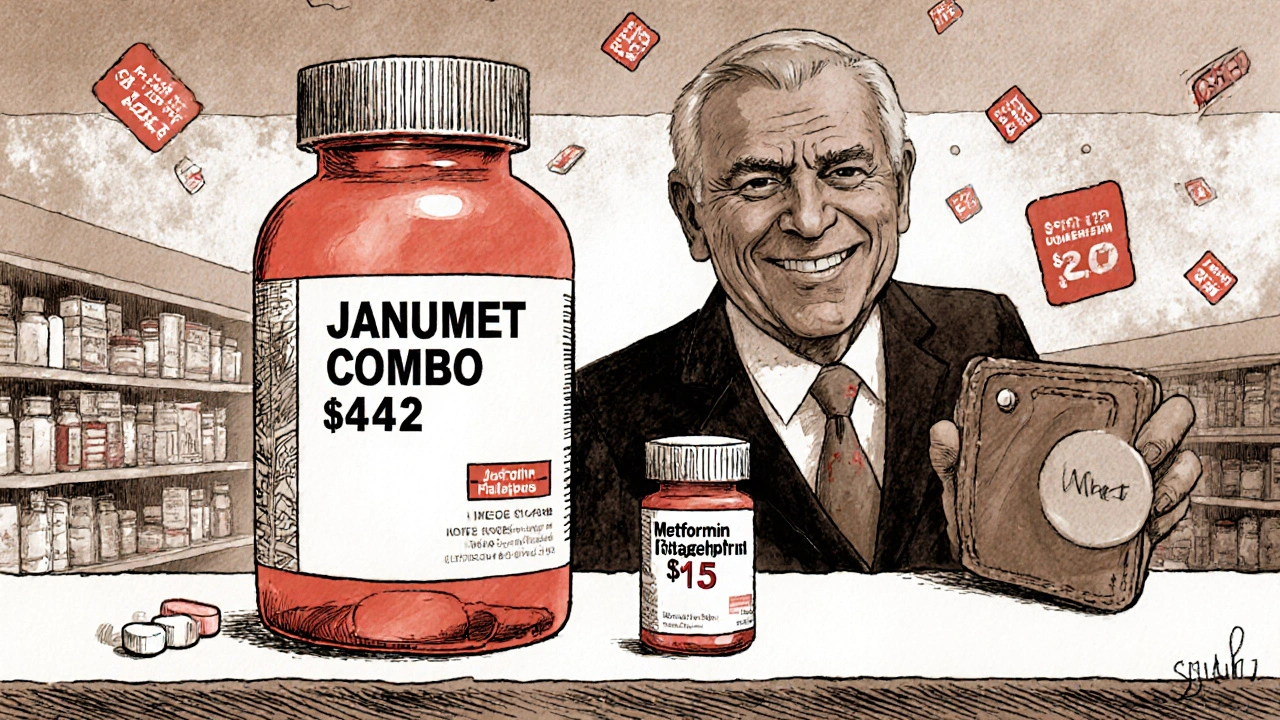
Fixed-dose combinations (FDCs) aren’t inherently expensive. The problem is when pharmaceutical companies combine a generic drug-like metformin, which costs $4 for a 30-day supply at Walmart-with a newer, still-patented drug, like sitagliptin. Then they sell the combo as a branded product for $472 a month.
That’s not innovation. That’s pricing strategy. It’s called “evergreening.” When a drug’s patent is about to expire, companies bundle it with another drug-often one that’s already generic-to extend their monopoly. The result? You pay 10 to 15 times more than you would if you bought the two pills separately.
Take Janumet: sitagliptin + metformin. The branded version costs about $472 per month. Generic metformin? $4. Generic sitagliptin? Not widely available yet, but even if you bought the brand-name sitagliptin alone, it’s still far cheaper than the combo. Same with Kazano: alogliptin + metformin. The combo runs $425 a month. Generic metformin? Less than $10.
The Math Doesn’t Add Up
Here’s how the pricing works in real life:
- Two separate generic pills: $10-$20/month
- Branded combo pill: $400-$500/month
That’s a 20x to 50x markup. And it’s not just Medicare paying. Private insurers, patients with high deductibles, and even those on Medicaid are getting hit with these inflated prices.
According to IQVIA, combo drugs typically cost 60% of what two branded pills would cost-but that’s still way more than the sum of two generics. In fact, when one component is generic and the other is brand-new, the combo often costs more than the new drug alone. That’s because manufacturers know patients and doctors will choose the convenience of one pill, even if it’s far more expensive.
Who’s Getting Screwed?
Patients aren’t the only ones losing. Medicare Part D pays 22-33% more for the same brand-name drugs than the Department of Veterans Affairs does. Why? Because VA negotiates prices directly. Medicare can’t-until recently.
The Inflation Reduction Act of 2022 finally gave Medicare the power to negotiate prices for a handful of the most expensive drugs. That’s a start. But combo drugs are still slipping through the cracks. Only a few are currently eligible for negotiation, and most combo drugs aren’t even on the list.
Meanwhile, pharmacy benefit managers (PBMs) and insurance plans are starting to push back. About 62% of Medicare Part D plans now require prior authorization before covering high-cost combos. That means your doctor has to prove you can’t use cheaper alternatives first. It’s a bureaucratic hurdle-but it’s also a sign that the system is catching on.
But What About Adherence?
Pharma companies argue that combo pills improve adherence. And they’re not totally wrong. Studies show people are 15-25% more likely to take one pill than two or three. That matters-especially for conditions like hypertension or diabetes, where skipping doses can lead to heart attacks, strokes, or kidney failure.
But here’s the catch: if the combo costs $400 and the generics cost $15, most people will skip the combo anyway. They can’t afford it. So the adherence benefit is only real for people who can pay. For the rest? They either go without, take the generic pieces separately, or end up in the ER because their blood sugar or blood pressure got out of control.
And here’s another thing: if you’re on Medicare, you can get your generic components filled at the same pharmacy. You don’t need a special prescription. Your pharmacist can split the combo into individual generics and bill them separately-sometimes even with no copay.
What You Can Do
Don’t assume the combo pill is your only option. Talk to your doctor and pharmacist. Ask:
- Are the individual components available as generics?
- How much would it cost if I bought them separately?
- Can you prescribe them as separate pills and still have them counted as a single regimen?
Many doctors don’t know the cost difference. They’re trained to think in terms of clinical guidelines, not pharmacy pricing. But if you bring the numbers to them-like showing a $425 combo versus a $12 generic alternative-they’ll often switch you over.
Some pharmacies even offer “splitting” services where they dispense the generic components in a single blister pack labeled as a combo. It’s the same convenience, without the markup.
The Bigger Picture
This isn’t just about pills. It’s about how the system is rigged. Combination drugs represent just 2.1% of prescriptions in Medicare Part D-but they account for 8.3% of total spending. That’s because they’re expensive, they’re marketed heavily, and they’re rarely challenged.
By 2027, combo drug sales are projected to hit $185 billion. Most of that growth will come from cardiovascular and diabetes meds-exactly the conditions where generics are widely available. That’s not progress. That’s exploitation.
And it’s not just in the U.S. In Europe, combo drugs like Nexlizet (ezetimibe/bempedoic acid) cost $12 a day-even though ezetimibe is generic and costs pennies. The manufacturer just tacked on the new drug and called it a day.
Bottom Line
Combo generics aren’t a myth. But branded combos with generic ingredients? They’re a financial trap. The convenience is real. The cost is not.
If you’re taking a combination drug, check the price of the individual components. You might be paying 50 times more than you need to. And if your doctor says it’s for adherence, ask: “Can I take the generics separately and still get the same benefit?” The answer is almost always yes.
The system isn’t broken. It’s working exactly as designed-for drug companies, not patients. But you have more power than you think. Ask the questions. Shop around. Push back. Your wallet-and your health-will thank you.
Are combo pills always more expensive than buying separate generics?
Not always-but in most cases where one component is generic and the other is still under patent, yes. For example, a combo pill with metformin and a newer diabetes drug can cost 10 to 50 times more than buying the two as separate generics. The only exceptions are when both components are still brand-name or when the combo includes a truly novel drug with no generic alternative.
Can I ask my pharmacist to split my combo pill into generics?
Yes. Pharmacists can often fill your prescription with the individual generic components and package them together in a blister pack labeled as a combo. This is called a “compound” or “split” prescription. It’s legal, safe, and commonly done in pharmacies that work with managed care organizations. Ask your pharmacist directly-it’s not something most doctors bring up, but it’s a standard option.
Why don’t doctors prescribe generics instead of combos?
Many doctors don’t know the price difference. They’re trained to focus on clinical guidelines, not pharmacy costs. Also, pharmaceutical reps push combo drugs because they’re more profitable. But if you bring them the numbers-like showing a $4 generic metformin versus a $472 combo-they’ll often switch your prescription. It’s not about what’s clinically better-it’s about what’s affordable.
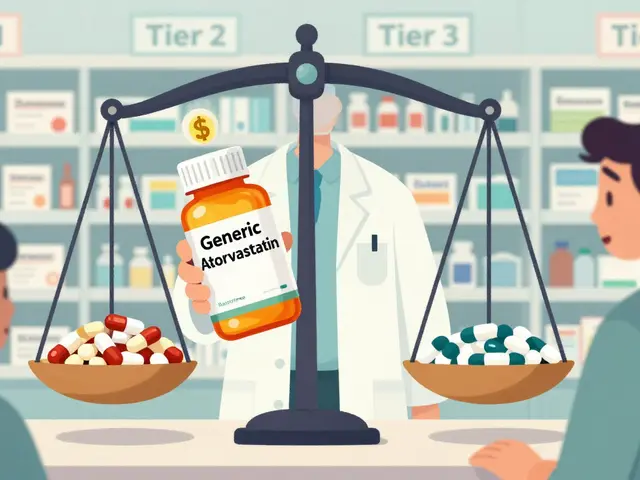
Does Medicare cover combo pills differently than separate generics?
Medicare Part D covers both, but many plans put combo pills in higher cost tiers. You might pay $50 for a combo pill but only $5 for the generics. Some plans require prior authorization for combos, meaning your doctor must prove you’ve tried cheaper options first. Always check your plan’s formulary before accepting a combo prescription.
Are there any combo drugs that are worth the extra cost?
Yes-but they’re rare. If both components are brand-new and have no generic alternatives, the combo might be justified. For example, some HIV or hepatitis C combos combine two novel antivirals that aren’t available separately. But for common conditions like high blood pressure, diabetes, or high cholesterol, the vast majority of combos are just repackaged generics with a premium price tag.


Comments
Bro. I was on Janumet for six months. $472 a month. My pharmacist looked me dead in the eye and said, "You’re literally paying for the packaging." I switched to metformin + sitagliptin generics. Paid $12. Same effect. Pharma doesn’t want you to know this. They want you addicted to the convenience. It’s not medicine-it’s a subscription service for rich CEOs.
they dont want you to know because they are in bed with the fda and the doctors are paid by big pharma to push these combos its all a scam the real cure is fasting and turmeric but no one wants to talk about that
Actually, the data is even more alarming than presented. According to the 2023 CMS Drug Spending Report, fixed-dose combinations account for 7.8% of total Part D expenditures despite representing only 2.1% of prescriptions-this is a textbook case of rent-seeking behavior enabled by regulatory capture. The fact that Medicare is prohibited from negotiating these prices until 2026 (and even then, only for 10 drugs) is a moral failure of legislative proportion.
USA still sleeping?? 😒 In Nigeria, we buy metformin for $0.50/month. Combo? $1.50. But here? $472?? This is capitalism at its most brutal. Pharma execs don’t even live here-they fly to Switzerland and laugh. We need a global revolt. 🚨💊 #PharmaIsTheNewColonialism
Interesting analysis. I’ve seen this in my pharmacy rotations-patients are often unaware that pharmacists can compound generics into a single blister pack. The real barrier isn’t clinical-it’s informational. Most prescribers aren’t trained in cost-aware prescribing. Maybe we need mandatory pharmacoeconomics modules in med school?
theyre using your blood pressure to fund their yachts and you dont even know it... the government is in on it too... the FDA approved these combos because they got paid... dont trust anything they say... the truth is hidden in plain sight
...and yet, nobody talks about the fact that PBMs are the real villains here... they take 20% of the rebate... then the pharmacy gets 5%... and the patient? They get the bill... it’s a pyramid scheme disguised as healthcare... and your doctor? They’re just the middleman... 😔
Man, I just told my uncle this last week. He was on a combo for diabetes, paying $500/month. I showed him the generic split. He cried. Said he’d been skipping doses because he couldn’t afford it. Now he’s on generics, takes them together in a pill organizer, and his HbA1c dropped from 9.2 to 6.8. It’s not magic-it’s just justice. 🙏
Back home in India, my dad takes metformin and lisinopril separately. Costs less than a cup of chai. Here? Same pills, same science, but you pay for the brand name like it’s a luxury watch. We need to stop romanticizing American healthcare. It’s not better-it’s just more expensive.
I never realized how much power I had until I asked my pharmacist about splitting my prescription. She looked at me like I was the first person who ever asked. I got my meds in a little blister pack labeled ‘Combo Pack’-same as the brand, but $14 instead of $450. I feel like I hacked the system. And honestly? It made me cry.
It’s heartbreaking, really. We talk about innovation in medicine, but this isn’t innovation-it’s exploitation dressed up as convenience. The fact that patients are being priced out of their own health care while executives get bonuses for ‘maximizing shareholder value’... it’s not capitalism. It’s a moral collapse. And the worst part? Most people just accept it because they don’t know any better.
Stop paying for lies.