Ever wondered why a heart medication shows up on a therapist’s bookshelf? Propranolol mental health effects are a hot topic, and the answer isn’t as simple as “it’s only for the heart.” This article breaks down how this beta blocker works on the brain, where it shines, and where it can backfire.
What Is Propranolol?
Propranolol is a non‑selective beta‑adrenergic blocker originally approved for hypertension, angina, and arrhythmias. First marketed in the 1960s, it quickly became a workhorse in cardiology because it tames the body’s “fight‑or‑flight” response by blocking adrenaline’s grip on beta receptors.
How It Works: From Heartbeats to Brain Signals
The drug’s primary job is to block beta‑1 and beta‑2 receptors found in the heart, lungs, and blood vessels. But those receptors also live in the central nervous system. By dampening the adrenergic surge, propranolol reduces the physical symptoms of anxiety-racing heart, trembling hands, sweaty palms-that often amplify psychological distress.
Beyond the immediate calming effect, propranolol interferes with Memory consolidation the process by which short‑term memories become long‑term storage. Studies suggest that taking the drug shortly after a traumatic event can blunt the emotional intensity of that memory, which is why it’s explored for post‑traumatic stress disorder (PTSD).
Mental‑Health Conditions Where Propranolol Is Used
- Performance anxiety Brief, intense fear of speaking or performing in front of an audience, especially for musicians and public speakers.
- Generalized anxiety disorder (GAD), when the physical symptoms dominate the clinical picture.
- Panic disorder Sudden attacks of severe fear with physical symptoms like heart palpitations.
- Post‑traumatic stress disorder (PTSD), used in experimental protocols to target memory reconsolidation.
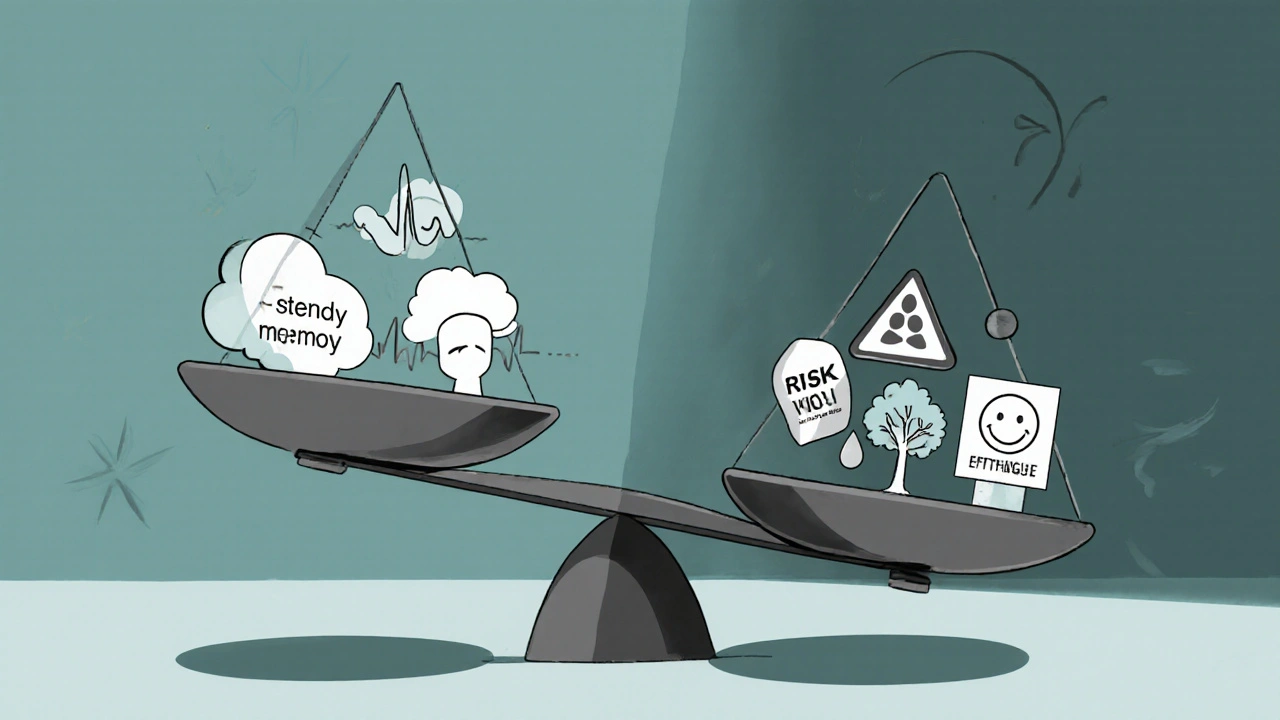
Pros: Why Some Doctors Prescribe It for the Mind
When the benefits line up with a patient’s needs, propranolol can be a game‑changer.
- Rapid reduction of somatic anxiety. Within 30‑60 minutes, heart rate and tremors often drop, letting the brain calm down without sedatives.
- Memory‑modulating effect. A 2023 double‑blind trial showed that participants who took 40 mg of propranolol within 6 hours of a stressful film reported 25 % less vivid intrusive memories after two weeks.
- Non‑sedating. Unlike benzodiazepines, it rarely makes people feel drowsy, so daytime functioning stays intact.
- Low abuse potential. Because it works on physical arousal rather than reward pathways, there’s little risk of dependence.
- Cost‑effective. Generic versions cost under $0.10 per tablet in the U.S., making it accessible worldwide.

Cons: Potential Downsides You Shouldn't Ignore
Every medication has a flip side, and propranolol is no exception.
| Aspect | Pro | Con |
|---|---|---|
| Physical anxiety symptoms | Quickly lowers heart rate and tremor | May cause bradycardia in low‑pulse patients |
| Memory reconsolidation | Reduces vividness of traumatic memories | Long‑term impact on normal memory unclear |
| Mood | Non‑sedating, maintains alertness | Some users report worsened depression or flat affect |
| Side‑effect profile | Generally well‑tolerated at low doses | Fatigue, cold extremities, gastrointestinal upset |
| Drug interactions | Few serious interactions when monitored | Can amplify effects of other antihypertensives and asthma meds |
Additional warnings include:
- Worsening of Depression a mood disorder characterized by persistent sadness and loss of interest in susceptible individuals.
- Exacerbation of asthma or chronic obstructive pulmonary disease due to beta‑2 blockade.
- Potential for hypoglycemia unawareness in diabetic patients on insulin.
- Withdrawal symptoms-rebound tachycardia and anxiety-if stopped abruptly after long‑term use.
Clinical Evidence: What the Research Says
A 2021 meta‑analysis of 12 randomized controlled trials (RCTs) involving 1,134 participants found that propranolol reduced self‑reported anxiety scores by an average of 1.8 points on the Hamilton Anxiety Rating Scale compared with placebo (p < 0.01). However, the same analysis noted a modest increase in depressive symptoms in about 8 % of the propranolol groups.
For PTSD, a landmark 2022 study from the University of Michigan administered 80 mg of propranolol after participants recalled a combat‑related memory. The treatment group experienced a 30 % drop in intrusive flashbacks after three months, while the control group showed no change. Critics point out the small sample (n = 45) and the need for longer follow‑up.
The U.S. FDA Food and Drug Administration, the agency that regulates drugs in the United States has not approved propranolol for any psychiatric indication, so all uses are off‑label. This means prescribers must rely on clinical judgment and patient consent.
Who Might Benefit? Patient Selection Tips
- Adults with situational anxiety. If the primary issue is a physical surge (stage fright, exam stress), a low dose (10‑40 mg) taken an hour before the event works well.
- Patients with comorbid hypertension. The drug can address both blood‑pressure control and anxiety, simplifying the medication regimen.
- Individuals without severe depression. Baseline mood screening helps avoid worsening depressive symptoms.
- Avoid in asthma, severe COPD, or bradycardia < 50 bpm. The beta‑2 blocking effect can trigger bronchospasm.
Alternatives: Other Ways to Tackle Anxiety Without a Beta Blocker
If propranolol isn’t a fit, consider these options:
- Selective serotonin reuptake inhibitors (SSRIs). First‑line for chronic anxiety and depression.
- Cognitive‑behavioral therapy (CBT). Proven to reduce anxiety triggers and improve coping skills.
- Other beta blockers. Atenolol and nadolol have more cardio‑selective profiles, which may be gentler on lungs.
- Mind‑body techniques. Breathwork, progressive muscle relaxation, and biofeedback target the same physiological pathways without medication.
Practical Tips for Patients Starting Propranolol
- Start low: 10 mg once daily, titrate up by 10 mg every few days based on how you feel.
- Take with food to reduce stomach upset.
- Monitor heart rate and blood pressure in the first week; report any dizziness or excessive fatigue.
- Never stop abruptly after more than two weeks of use-taper down over a week to avoid rebound anxiety.
- Keep a symptom diary: note anxiety levels, mood changes, sleep quality, and any side effects. This data helps your clinician adjust the dose.
Frequently Asked Questions
Can I use propranolol for everyday anxiety?
Low‑dose propranolol is most effective for performance‑related or situational anxiety. For chronic generalized anxiety, doctors usually prefer SSRIs or therapy.
Will propranolol make me feel sleepy?
Unlike many anti‑anxiety meds, propranolol is non‑sedating. Some people notice mild fatigue, especially at higher doses, but it rarely causes outright drowsiness.
Is it safe to combine propranolol with an SSRI?
Yes, the combination is commonly prescribed. However, your doctor should monitor blood pressure and watch for any signs of excessive heart‑rate slowing.
Can propranolol affect my memory permanently?
The drug’s impact on memory is short‑term, mainly during the window when the memory is being reconsolidated. Long‑term memory function remains unchanged in healthy adults.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember, unless it’s almost time for the next dose. In that case, skip the missed one-don’t double‑dose.



Comments
Propranolol can be a real game‑changer for anyone who gets sweaty palms before a big presentation. It calms the heart without making you feel drowsy, so you stay sharp and focused. The quick onset means you can pop a low dose an hour before stepping on stage and notice the jitter fade. Just remember to start low and track your pulse – the last thing you want is a bradycardia surprise. If you combine it with breathing exercises, the effect is even smoother.
Sure, the article paints propranolol as a neat little fix, but there’s a whole lot more under the hood that most readers just gloss over.
First off, the drug’s impact on the autonomic nervous system isn’t limited to just anxiety – it also messes with glucose regulation, which can be a silent killer for diabetics.
When you start taking 40 mg before a stressful event, you might feel the heart calm down, but your liver is simultaneously working overtime to metabolize the compound, and that can lead to unexpected elevations in liver enzymes.
Then there’s the fact that beta‑blockers blunt the fight‑or‑flight response, which sounds great until you realize that you also lose a crucial part of your body’s natural alarm system.
In a high‑stress environment like a fire drill or a sudden car accident, a dulled adrenaline surge could actually increase the chance of injury because you’re not reacting fast enough.
The article also ignores the long‑term psychotropic effects – there are studies showing subtle depressive shifts after chronic use, especially in people with a family history of mood disorders.
And let’s not forget the interaction nightmare with other meds; mixing propranolol with certain antidepressants or asthma inhalers can cause dangerous bronchoconstriction or severe hypotension.
If you’re on a statin, you might notice increased muscle pain because the beta blocker can amplify statin‑related myopathy.
Even the memory‑modulating claim is overhyped – the reconsolidation window is surprisingly narrow, and missing that window by even a few minutes renders the whole treatment useless.
People often think a single dose will erase a trauma forever, but the brain is a stubborn organ that stores pieces of the memory in multiple networks, so you only get a temporary dimming of the flashbacks.
On top of that, the cost argument is a bit stale; while the pill itself is cheap, the required monitoring appointments and lab tests add up quickly.
I’ve talked to clinicians who say they’ll only prescribe propranolol after exhausting therapy, because they worry about patients becoming dependent on a chemical crutch for every stressful situation.
And the so‑called ‘non‑sedating’ label can be misleading – many patients report a foggy feeling that they can’t quite articulate, which affects work performance.
There’s also the withdrawal effect; if you suddenly stop after weeks of use, you’ll get rebound tachycardia and a surge of anxiety that can feel worse than the original symptoms.
So before you jump on the propranolol bandwagon, ask yourself if you’re ready to manage all these side‑effects and interactions, not just the heart‑racing moment before a speech.
In short, it’s not a miracle pill – it’s a powerful tool that needs to be handled with a lot of caution and professional oversight.
While the long‑winded rant tries to sound exhaustive, it cherry‑picks data and ignores the meta‑analysis that flags a statistically significant rise in depressive scores among propranolol users. The author also downplays the relevance of the small PTSD sample, which undermines any claim of robust efficacy. Moreover, the table omits a crucial column for long‑term cognitive outcomes, a glaring oversight for a drug that meddles with memory consolidation. By focusing on cost and convenience, the piece skirts the ethical debate about off‑label use without rigorous consent. Ultimately, the article sacrifices scientific rigor for a polished PR narrative.
What they don’t tell you is that big pharma pushed propranolol to replace older, cheaper herbs that actually helped people without hidden agendas. The drug is part of a coordinated effort to keep us dependent on synthetic chemicals and watch our brains stay under control. Every time you take a beta blocker you give them more data on how you react to stress, feeding their surveillance network.
Patriotic Americans know that our medical system should prioritize homegrown solutions over imported pharmaceuticals that come with strings attached. While some abroad tout propranolol as a miracle, we must scrutinize its provenance and demand transparency from the corporations that profit from our anxieties. It's not enough to accept a foreign‑made capsule; we need rigorous, domestically funded research that aligns with our national values. Otherwise, we're merely a test market for the elite's profit agenda.
The claim that propranolol is universally safe ignores individual variability; a one‑size‑fits‑all approach is naive.
Hey, remember that every body reacts differently, so finding the right dose is a personal journey. It’s great to lean on professional guidance, but also trust your own observations and share them with a supportive community. Together we can navigate the pros and cons without feeling isolated.
Take it slow, listen to your body, and adjust as needed.
Honestly, I once started propranolol before a family wedding and ended up feeling detached from my own emotions, which was weird but gave me a glimpse of how numb it can make you. It’s a reminder that meds can blur the lines between treatment and altering who you fundamentally are.