When people hear the term inflammatory bowel disease, they often think of one condition. But IBD isn’t one thing-it’s two very different diseases that look similar on the surface but behave in completely different ways. Crohn’s disease and ulcerative colitis both cause chronic gut inflammation, pain, and fatigue. Yet how they develop, where they strike, and how they’re treated can be worlds apart. Knowing the difference isn’t just academic-it changes your treatment plan, your prognosis, and even your daily life.
Where the Inflammation Happens
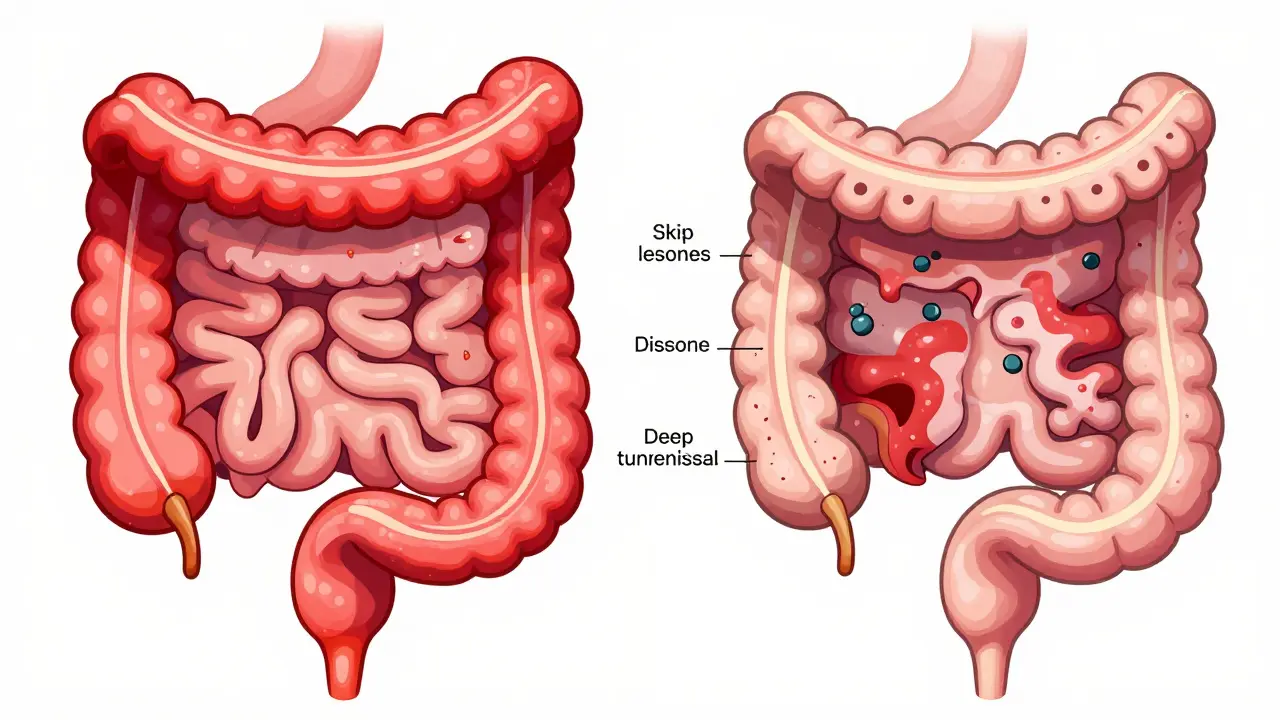
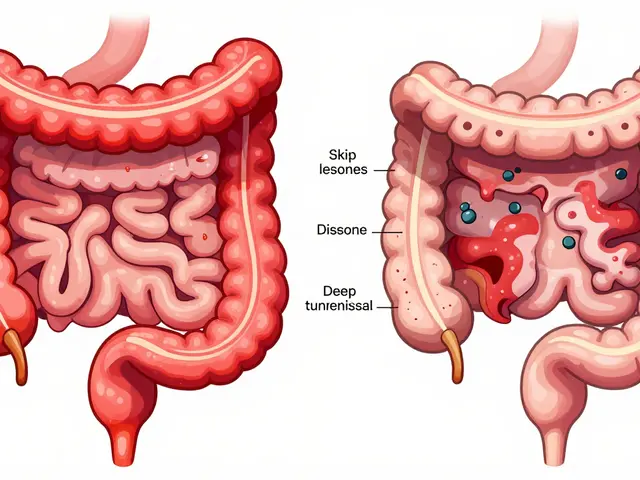
- Ulcerative colitis only affects the colon and rectum. It starts at the rectum and spreads upward in a continuous line. If you have UC, your entire colon might be inflamed-or just the lower part. But it never touches the small intestine.
- Crohn’s disease can show up anywhere from your mouth to your anus. Most often, it hits the end of the small intestine (ileum) and the beginning of the colon. But it can also appear in patches, skipping healthy sections of bowel. This is called "skip lesions," and it’s a hallmark sign of Crohn’s.
This difference in location isn’t just a map detail-it affects what symptoms you feel. People with ulcerative colitis often have urgent, bloody diarrhea because the rectum is always involved. Crohn’s patients might have pain around the belly button or lower right side, especially if the ileum is inflamed. Some even develop mouth sores or anal fissures, which are rare in UC.
How Deep the Damage Goes
Ulcerative colitis stays on the surface. It only eats away at the innermost layer of the colon wall-the mucosa. That’s why bleeding is so common. It’s like a sunburn on the inside of your gut.
Crohn’s disease? It goes all the way through. This is called transmural inflammation. It hits the mucosa, then the muscle layer, and sometimes even the outer membrane. That’s why Crohn’s can lead to complications like fistulas-abnormal tunnels between organs-and strictures, which are narrow, scarred sections of intestine that block food.
Think of it this way: UC is a shallow cut. Crohn’s is a deep wound that can tunnel under the skin. That’s why surgery for UC can be curative, but surgery for Crohn’s is rarely a permanent fix.
What Tests Reveal
There’s no single blood test that tells you which one you have. Colonoscopy is the gold standard. Here’s what doctors look for:
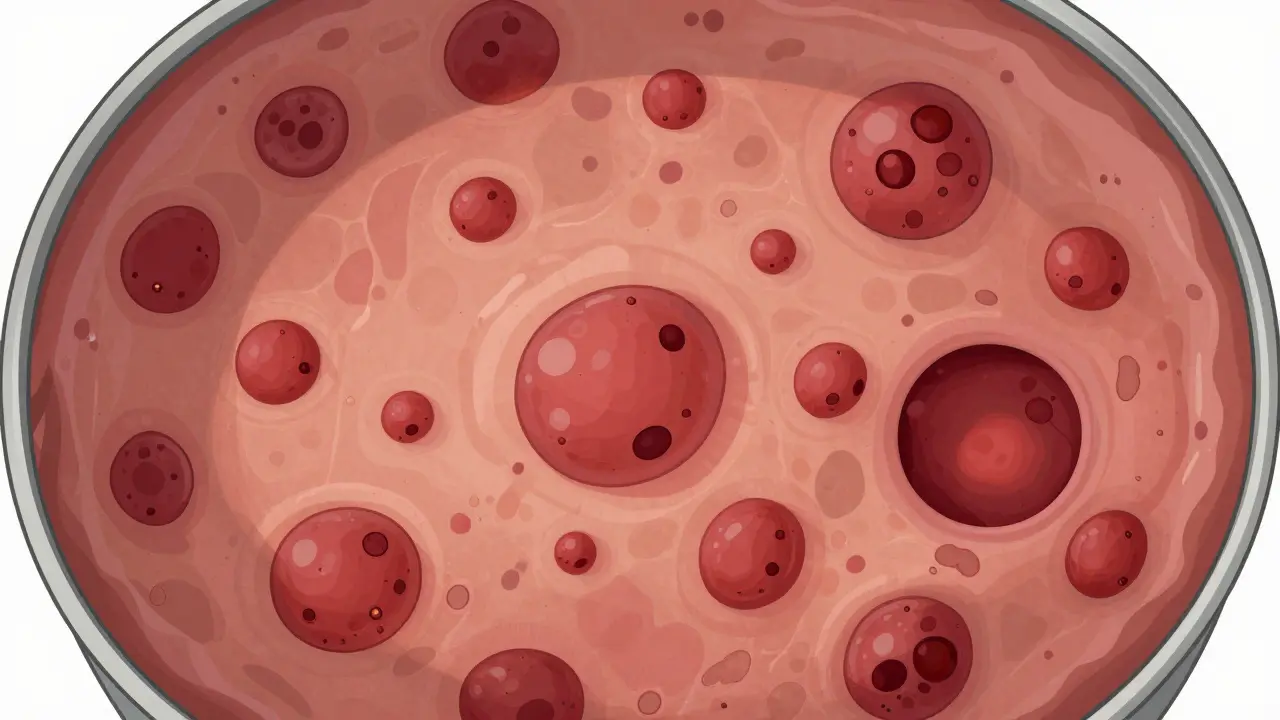
- For ulcerative colitis: Continuous redness, ulcers, and bleeding starting at the rectum. Pseudopolyps-small bumps of healing tissue-often form. Biopsies show inflammation only in the top layers.
- For Crohn’s disease: Patchy inflammation with healthy tissue in between. The lining looks like cobblestones. Deep ulcers, fistulas, and thickened bowel walls are visible. Sometimes, even the small intestine needs to be checked with a capsule endoscopy or MRI enterography.
Blood and stool tests help too. A high level of fecal calprotectin means active inflammation-but it doesn’t tell you which disease. The pANCA blood test is positive in 60-70% of UC patients but only 10-15% of Crohn’s patients. That’s a useful clue, though not definitive.
Complications Are Not the Same
Both conditions raise your risk of colon cancer over time, but other complications are very different.
- Crohn’s disease: About 1 in 3 people develop strictures. 1 in 4 get fistulas-some connect the bowel to the bladder, skin, or vagina. These often need surgery or biologics to heal.
- Ulcerative colitis: Toxic megacolon is rare but deadly. It’s when the colon suddenly swells and stops working. It happens in about 5% of severe flares. Also, 3-7% of UC patients develop primary sclerosing cholangitis, a serious liver disease that doesn’t occur in Crohn’s.
Extraintestinal symptoms like joint pain, skin rashes, and eye inflammation affect about a third of all IBD patients, regardless of type. But the liver issue? That’s almost exclusive to UC.
Treatment Approaches Diverge
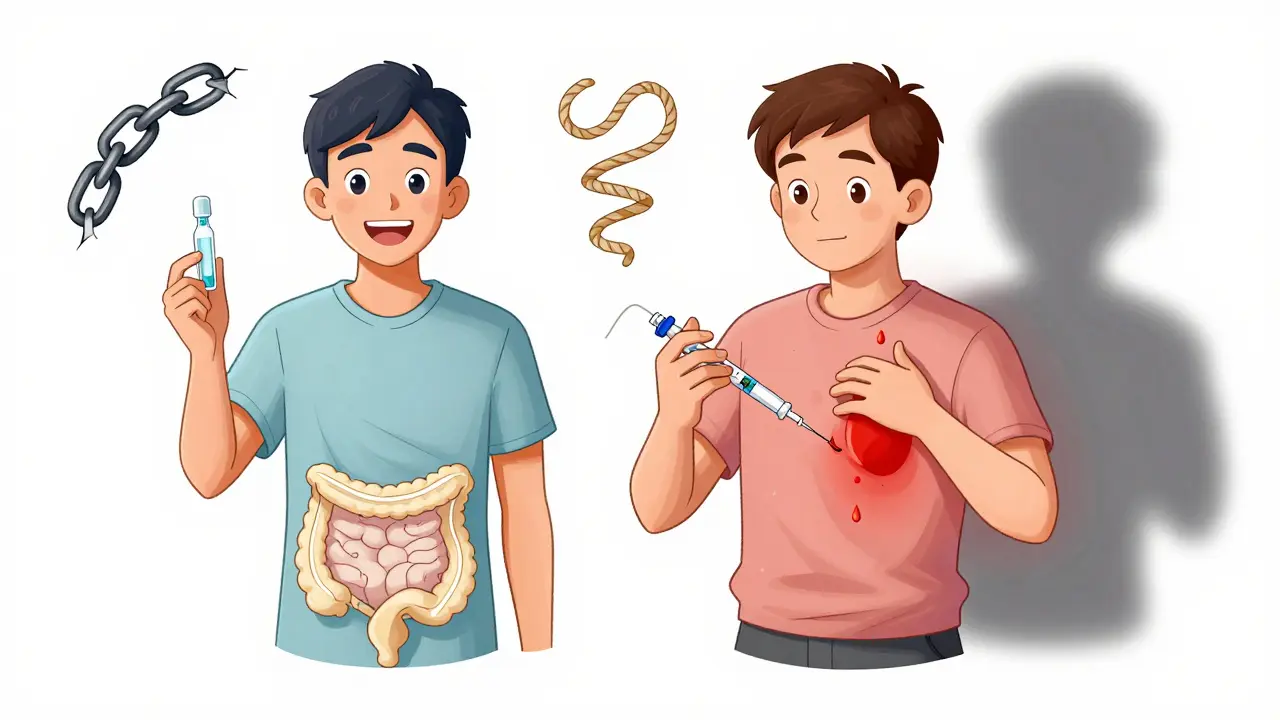
Both conditions use anti-inflammatory drugs and immune suppressors, but the strategy changes based on location and depth.
- Ulcerative colitis: Topical treatments work well. Enemas and suppositories with 5-ASA drugs deliver medication right to the inflamed colon. For moderate to severe cases, biologics like vedolizumab target gut-specific immune cells. Surgery-removing the entire colon and rectum-is the only true cure.
- Crohn’s disease: Since it can affect the whole GI tract, systemic drugs are needed. Oral immunomodulators like azathioprine or biologics like infliximab are common. Surgery removes damaged sections, but the disease almost always comes back nearby. That’s why it’s not called a cure.
Interestingly, anti-TNF drugs (like Humira or Remicade) work better for Crohn’s than for UC. In clinical trials, 30-40% of Crohn’s patients went into remission after 54 weeks, compared to 20-30% of UC patients.
Surgery: Cure or Temporary Fix?
This is one of the biggest differences.
If you have ulcerative colitis and your symptoms are out of control, removing your colon and rectum can end the disease forever. Surgeons can create a pouch from the small intestine and attach it to the anus. Most people regain normal bowel function. About 10-15% of UC patients end up having this surgery within 10 years.
For Crohn’s, surgery is a last resort. You might have a piece of bowel removed, but the disease comes back in 50% of cases within 10 years. That’s because the problem isn’t just the tissue-it’s your immune system. Removing the damaged part doesn’t fix the root cause.
What Patients Actually Experience
Real-world data from thousands of IBD patients shows clear patterns:
- 75% of UC patients report frequent rectal bleeding. Only 35% of Crohn’s patients do.
- 87% of UC patients feel sudden, urgent bowel movements. For Crohn’s, it’s 68%.
- Crohn’s patients are twice as likely to struggle with weight loss and nutrient deficiencies. That’s because the small intestine, where nutrients are absorbed, is often affected.
- On patient forums, UC patients say stress triggers their flares. Crohn’s patients point to specific foods-dairy, high-fiber veggies, or greasy meals.
These aren’t just anecdotes. A 2023 survey of 1,200 IBD patients confirmed these trends. If you’re trying to manage your symptoms, knowing which disease you have helps you avoid your personal triggers.
When It’s Not Clear
Not every case fits neatly. About 10-15% of people are initially diagnosed with "indeterminate colitis." Their symptoms and test results don’t clearly point to Crohn’s or UC. In these cases, doctors watch and wait. Over time, some patients develop features that confirm one diagnosis. A Swiss study found that 12.3% of people initially labeled as UC later turned out to have Crohn’s, because they developed fistulas or strictures.
That’s why follow-up is critical. A diagnosis isn’t always final.
What’s Next for IBD Treatment
New therapies are emerging. Fecal microbiota transplants (FMT)-essentially a poop transplant-have shown 32% remission rates in UC patients in recent trials. But for Crohn’s, the same treatment only worked in 22%. That suggests the gut microbiome plays a different role in each disease.
Drugs like mirikizumab (for Crohn’s) and etrolizumab (for UC) are in late-stage trials. Both target specific immune pathways, but they’re designed for different disease behaviors. The FDA is expected to make decisions by late 2024.
One thing is clear: treatment is becoming more personalized. It’s not just about which disease you have-but how it’s behaving. Is it inflamed? Narrowed? Fistulizing? That’s now more important than whether it’s labeled Crohn’s or UC.
Can you have both Crohn’s disease and ulcerative colitis?
No, you can’t have both at the same time. They are two distinct diseases. But about 10-15% of people are initially diagnosed as having "indeterminate colitis" because their symptoms and test results don’t clearly match either condition. Over time, as the disease progresses, doctors can usually reclassify it as either Crohn’s or UC based on new symptoms or complications.
Is one disease worse than the other?
Neither is "worse"-they’re just different. Crohn’s disease tends to have more unpredictable complications like fistulas and strictures, which can require multiple surgeries. Ulcerative colitis has a higher risk of toxic megacolon and colon cancer over time. But UC can be cured with surgery, while Crohn’s cannot. The severity depends on how deeply the disease affects your body, not just the label.
Do diet and stress cause IBD?
No, diet and stress don’t cause Crohn’s disease or ulcerative colitis. Both are autoimmune conditions triggered by a mix of genetics, immune system dysfunction, and environmental factors like antibiotics or gut microbiome changes. But once you have IBD, certain foods and high stress can trigger flares. For example, dairy often worsens Crohn’s symptoms, while stress is a top trigger for UC flares.
Can IBD be cured?
Ulcerative colitis can be cured with surgery-removing the entire colon and rectum. After that, the disease is gone for good. Crohn’s disease cannot be cured. Even if you have surgery to remove damaged sections, the disease almost always returns nearby. The goal with Crohn’s is long-term remission, not elimination.
Why do some people with IBD need biologics?
Biologics are targeted drugs that block specific parts of the immune system causing inflammation. They’re used when standard treatments like 5-ASAs or steroids don’t work. For Crohn’s, anti-TNF drugs (like infliximab) help about 30-40% of patients. For UC, newer biologics like vedolizumab target gut-specific immune cells and work well for many who don’t respond to other drugs. They’re not cures, but they can put the disease into deep remission.