Imagine you’re taking a statin to lower your cholesterol, and then you get a stubborn yeast infection or toenail fungus. Your doctor prescribes an antifungal like fluconazole or itraconazole. Sounds straightforward, right? But here’s the hidden danger: statins and certain antifungals can clash in your body in ways that could land you in the hospital.
Why This Interaction Isn’t Just a Minor Warning
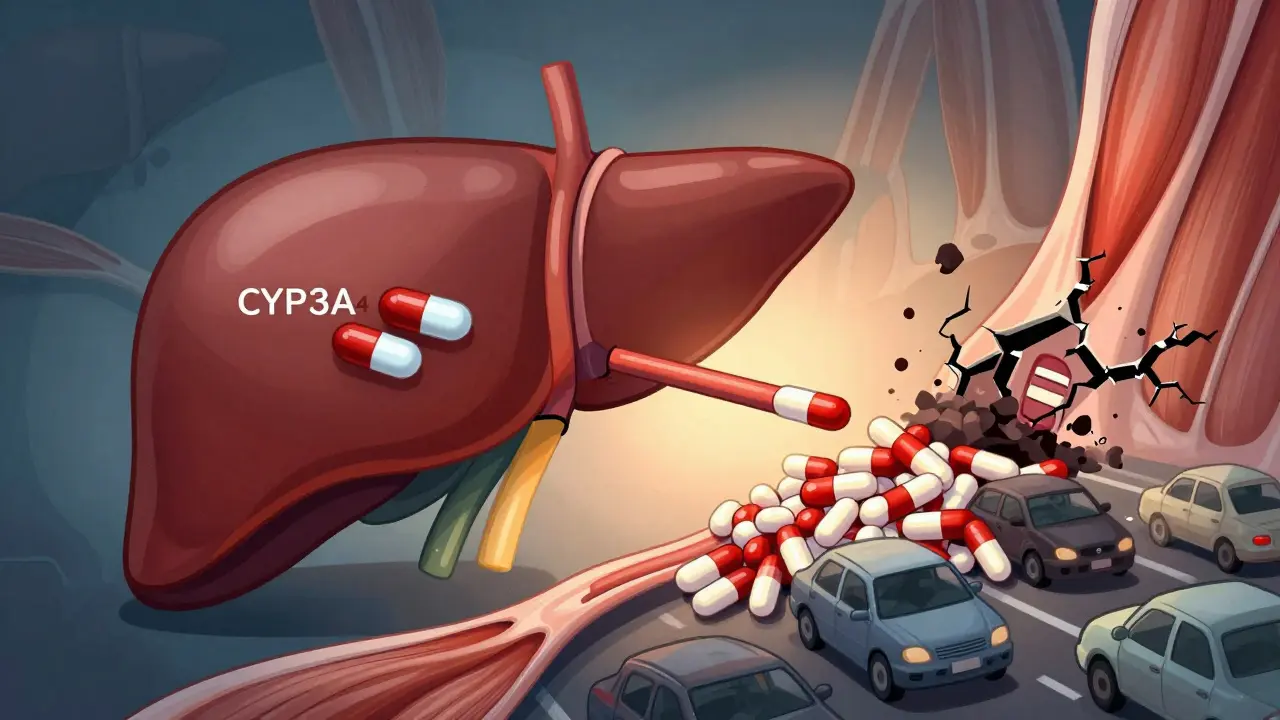
Statins like simvastatin, atorvastatin, and lovastatin work by blocking an enzyme in your liver that makes cholesterol. But they also rely on your liver’s CYP3A4 enzyme to break them down and clear them from your system. That’s where azole antifungals - fluconazole, itraconazole, ketoconazole, voriconazole - come in. These drugs don’t just kill fungi. They also slam the brakes on CYP3A4, the very enzyme your body needs to process statins. When that happens, your statin doesn’t get cleared. It builds up. And when levels get too high, your muscles start breaking down. That’s called rhabdomyolysis. It’s rare, but when it happens, it’s serious. Your muscles turn to debris, your kidneys get overwhelmed, and you could end up needing dialysis. One case report in the BMJ showed simvastatin levels spiking tenfold when taken with itraconazole. Muscle pain? That’s not just soreness. It’s your body screaming for help.Not All Statins Are Created Equal
Here’s the good news: not every statin carries the same risk. Your body handles different statins in different ways.- High-risk statins: Simvastatin, lovastatin, and atorvastatin. These are mostly broken down by CYP3A4. If you’re on one of these and get prescribed an azole antifungal, you’re in the danger zone.
- Moderate-risk: Fluvastatin. It’s processed by CYP2C9, which fluconazole can also inhibit - so caution still applies.
- Low-risk statins: Pravastatin and rosuvastatin. These mostly leave your body unchanged through your kidneys. They don’t rely on CYP3A4. That makes them the safer choice if you need an antifungal.
So if you’re on simvastatin and your doctor suggests itraconazole for a fungal infection, that’s not a routine swap. That’s a red flag. The FDA explicitly warns against combining simvastatin with itraconazole. And yet, pharmacists report catching 10 to 12 of these dangerous combos every quarter - often for something as simple as toenail fungus.
Real Stories, Real Consequences
On patient forums, the stories are chilling. One user on the American Heart Association’s support site, ‘CholesterolWarrior42,’ described severe muscle pain after starting fluconazole for a yeast infection while on simvastatin. Their creatine kinase (CK) levels - a marker of muscle damage - hit over 15,000 U/L. Normal is under 200. They ended up in the ER. Another Reddit user, a pharmacist named ‘MedSafetyFirst,’ said they’ve stopped at least 12 dangerous prescriptions this year alone, mostly involving simvastatin and itraconazole for fungal nails. But it’s not all bad news. A 2022 survey by the National Lipid Association found that 87% of patients who switched to pravastatin or rosuvastatin during antifungal treatment had no issues with their cholesterol control. The key? Planning ahead.
What You Should Do If You Need Both
If you’re on a statin and your doctor says you need an antifungal, here’s your action plan:- Ask if the infection can be treated topically. For athlete’s foot or yeast infections on the skin, creams or sprays like clotrimazole or terbinafine work just as well - and they don’t get into your bloodstream enough to cause interactions.
- Ask for a different antifungal. Terbinafine doesn’t interfere with CYP3A4. It’s a great alternative for fungal nails or skin infections.
- Ask if you can switch statins. If you’re on simvastatin or lovastatin, ask if you can temporarily switch to pravastatin or rosuvastatin during antifungal treatment. It usually takes 3 to 5 days for the old statin to clear out.
- If you can’t switch, pause the statin. Some experts recommend stopping your statin 2 days before starting the antifungal and waiting 2 days after finishing it. This isn’t always practical, but it’s safer than risking rhabdomyolysis.
And never assume your doctor knows. A 2023 study in JAMA Internal Medicine found only 42% of primary care doctors could correctly identify which statin-azole combos were dangerous. You might be the only one who catches it.
The Surprising Upside: Statins Might Help Fight Fungi
Here’s something you won’t hear in most doctor’s offices: statins might actually help antifungals work better. Research shows that when statins like fluvastatin and atorvastatin are combined with azoles, they can boost the drug’s ability to kill stubborn fungi like Candida auris - a superbug that’s become a nightmare in hospitals. In lab studies, these combinations lowered the amount of antifungal needed to kill the fungus by up to 80%. That’s why researchers are now running clinical trials - like the NIH-funded STATIN-AF trial - to see if low-dose statins can be used as a treatment boost for drug-resistant fungal infections. The goal? To turn a dangerous interaction into a powerful therapy.

Comments
Wow. I just got prescribed fluconazole last week for a yeast infection and I’m on simvastatin. I’m gonna call my pharmacist first thing tomorrow. This post saved me from a nightmare.
Thanks for laying it out so clearly. I didn’t even know statins and antifungals could do this. 🙏
Of course this is a problem. Big Pharma doesn’t want you to know this stuff. They profit off the side effects. Rhabdomyolysis? That’s not a side effect - that’s a business model.
And don’t get me started on how doctors are trained to trust labels, not biology. They’re just following the script. You’re on your own.
I had muscle pain for weeks last year and didn’t connect it to my meds. I thought I was just getting old. This is so important. Please share this with everyone you know. People need to know.
Ugh. Another ‘warning’ article. Like we don’t already know drugs are dangerous? I’ve been on statins for 12 years and never had an issue. Why are we being scared into switching meds? This is fearmongering disguised as medicine.
Also - terbinafine? That’s for fungi. I don’t need some ‘natural’ fix. I need science. Not hippie nonsense.
I’m so tired of how medicine treats patients like disposable data points. You get a statin because you’re ‘high risk’ - then you get an antifungal because you’re ‘unlucky’ - and suddenly your body is a warzone with zero consent.
It’s not just the drugs. It’s the silence. The assumption that we won’t ask. That we won’t fight.
Thank you for giving us the words to fight back.
This is exactly the kind of information that should be taught in every high school health class. Not just ‘take your pills’ - but ‘know why they work, and when they might hurt you.’
If you’re on a statin and need an antifungal, please don’t panic. Just pause. Call your pharmacist. Ask about pravastatin. It’s a simple switch - and it could save your kidneys.
You’ve got this. And you’re not alone.
OMG I just read this and immediately checked my meds - I’m on atorvastatin and was about to start fluconazole for a recurring rash. I canceled my prescription and called my doctor. Thank you so much for this!! 🙌❤️
Also, the part about statins helping fight fungi? Mind blown. Science is wild.
Wait so if I’m on simvastatin and my doctor gives me itraconazole… I should just say NO? Like, flat out? What if they get mad? 😬
People need to stop acting like their doctor is a god. If your doctor doesn’t know this interaction, they’re not qualified to prescribe statins. Period. I’ve seen too many people get hurt because they trusted the white coat instead of their gut.
Ask. Push. Demand answers. You’re not being difficult - you’re being responsible.
Statins help fight fungi? That’s the dumbest thing I’ve heard all week. If statins were antifungal, we’d just give everyone statins and call it a day. This is just another ‘scientists are secretly genius’ fairy tale.
As someone who has published three peer-reviewed papers on CYP3A4 pharmacokinetics, I must say this article is dangerously oversimplified. The risk of rhabdomyolysis with fluconazole and atorvastatin is negligible in healthy patients under 65 - it’s primarily a concern with polypharmacy, renal impairment, or genetic polymorphisms in SLCO1B1.
Furthermore, the NIH’s STATIN-AF trial is still Phase II. The 80% reduction in antifungal MICs is in vitro - not clinically validated. To present this as a therapeutic strategy is misleading at best.
And yet, the article’s tone - emotional, alarmist, anecdotal - will cause more harm than good. Patients will discontinue essential statins. Cholesterol will rise. Cardiovascular events will increase.
Science is not a headline. It is nuance. And this post, despite its good intentions, is a disservice to public health.
bro i live in india and my doctor gave me itraconazole for nail fungus and i was on rosuvastatin... no problem. but i know people here who take statins from the pharmacy without prescription. they dont even know what cyp3a4 is. this is why we need better education. not just in usa.
also terbinafine is cheaper here. like 20 rupees. why pay more?
USA thinks it owns medicine. In India we’ve been using terbinafine for decades. No alerts. No panic. Just common sense. Why do you need an app to tell you not to mix pills? Your body isn’t a computer. Stop overcomplicating everything.
Wait so if I switch to pravastatin, will it still help my cholesterol? I’m scared to change anything. 😅