Why Your Kidneys Need a Special Diet
When your kidneys aren’t working right, they can’t filter out extra salt, potassium, and phosphorus like they should. These minerals build up in your blood, and that’s dangerous. Too much sodium makes you retain fluid, raising your blood pressure and straining your heart. High potassium can mess with your heartbeat - even cause it to stop. Too much phosphorus pulls calcium from your bones and hardens your arteries. A renal diet isn’t about eating less food. It’s about eating smarter.
Sodium: The Hidden Enemy in Processed Foods
Most people don’t realize they’re eating way too much sodium. In the U.S., 75% of sodium comes from packaged and restaurant foods, not from the salt shaker. For someone with chronic kidney disease (CKD), the goal is to stay under 2,000-2,300 mg per day. That’s about one teaspoon of table salt - but you’re not just avoiding salt. You’re avoiding everything that’s been preserved, cured, or flavored with it.
Look at the labels. One can of soup can have 800-1,200 mg of sodium. A single slice of processed cheese? Around 400 mg. Deli meats, frozen meals, canned beans, and even bread are loaded. Even "low-sodium" products can be deceptive - check the serving size. Instead, choose fresh meats, plain frozen vegetables, and unseasoned rice or pasta. Cook at home. Use herbs like rosemary, thyme, or garlic powder instead of salt. Mrs. Dash and other salt-free blends work well. Cutting sodium by just 1,000 mg a day can drop your systolic blood pressure by 5-6 mmHg, according to the CDC.
Potassium: The Balancing Act
Potassium is essential for muscle and nerve function, but your kidneys need to be healthy to remove the excess. When they’re not, potassium builds up. Levels above 5.5 mEq/L can trigger dangerous heart rhythms. The target for most stage 3-5 CKD patients is 2,000-3,000 mg per day, but your doctor will adjust this based on your blood tests.
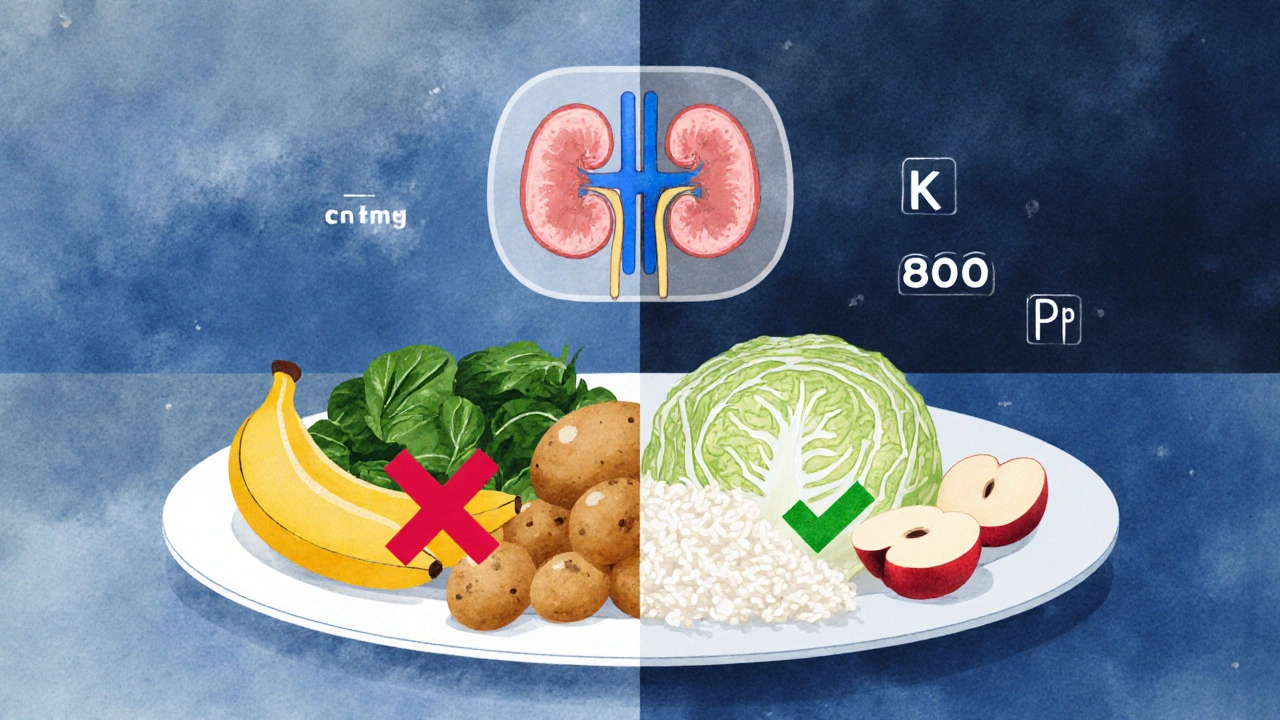
High-potassium foods are often the ones you think of as healthy: bananas (422 mg each), oranges (237 mg), potatoes (926 mg per medium), tomatoes, spinach, and avocado. These need to be limited or avoided. But you don’t have to give up fruits and veggies entirely. Portion control matters. A half-cup of blueberries has only 65 mg of potassium. An apple has 150 mg. Cabbage? Just 12 mg per half-cup cooked. Leaching vegetables - soaking them in warm water for 2-4 hours, then boiling them in plenty of water - can cut potassium by up to 50%. DaVita’s 2023 nutrition guide shows this technique works for potatoes, carrots, and beets. Also, remember: potassium from animal foods (meat, dairy) is absorbed more easily than from plants. So even if a plant is high in potassium, your body might not absorb it all.
Phosphorus: The Silent Bone Thief
Phosphorus is where things get tricky. Your body absorbs natural phosphorus from foods like meat, dairy, and nuts at about 50-70%. But the phosphorus added to processed foods - in colas, processed cheeses, deli meats, and baked goods - is absorbed at 90-100%. That’s why dietitians say it’s not the amount of phosphorus you eat, but where it comes from.
For non-dialysis CKD patients, the goal is 800-1,000 mg per day. A 12-ounce cola has 450 mg. One slice of processed cheese? 250 mg. A glass of milk? 125 mg. Whole-grain bread? 150 mg per slice. White bread? Only 60 mg. That’s why swapping whole-grain for white bread, or choosing rice milk over cow’s milk, makes a big difference. Some foods are now being specially formulated to help - like phosphate-binding rice developed in 2023 and tested in clinical trials. And yes, there’s controversy. The European Renal Association says restricting phosphorus below 1,200 mg/day doesn’t necessarily improve survival in non-dialysis patients. But most U.S. nephrologists still follow the tighter KDOQI guidelines, especially if your blood phosphorus is high.
What to Eat: Real Food Examples
Here’s what a day might look like on a renal diet:
- Breakfast: White toast (2 slices, 120 mg phosphorus), scrambled eggs (1 whole + 2 whites), apple slices (150 mg potassium), coffee with non-dairy creamer
- Lunch: Grilled chicken breast (3 oz, low sodium), white rice, steamed cabbage (leached), pear (1 small, 190 mg potassium)
- Dinner: Baked cod (3 oz, low sodium), mashed cauliflower (leached), green beans (½ cup, 130 mg potassium), water
- Snacks: Rice cakes, unsalted popcorn, a few strawberries (100 mg potassium)
Fish like salmon, cod, halibut, and tuna are good protein choices - low in sodium, moderate in potassium and phosphorus. Stick to 2-3 ounce portions, 2-3 times a week. Avoid canned tuna in brine - rinse it well or choose water-packed. Skip the deli meats. Don’t drink soda - even diet colas have phosphorus additives. Water, herbal teas, and lemon water are your best fluid choices.
Why This Diet Works - And When It Doesn’t
Research shows a well-managed renal diet can delay the need for dialysis by 6-12 months in stage 4 CKD patients, according to Dr. Linda Fried at Columbia University. But it’s not a one-size-fits-all. The KDIGO 2023 guidelines now stress individualization. Some people need stricter limits; others can be more flexible. What’s critical is avoiding protein over-restriction. Earlier advice pushed for very low protein diets, but Dr. Srinivasan Beddhu’s 2022 study found that eating less than 0.6g of protein per kg of body weight increased malnutrition risk by 34% in older adults. Current guidelines recommend 0.55-0.8g/kg/day of high-quality protein - enough to maintain muscle, not enough to overload your kidneys.
Also, don’t forget fluid intake. If you’re producing less than 1 liter of urine a day, you may need to limit fluids to 32 oz (about 1 liter). This includes soups, ice, and even gelatin. Too much fluid leads to swelling, shortness of breath, and heart strain.

Tools and Support That Help
Managing this diet is hard. Most people take 3-6 months to adjust. The biggest hurdle? Taste. Food feels bland at first. But your palate resets. You start noticing natural flavors again. Registered dietitians who specialize in kidney care are your best allies. Medicare now covers 3-6 sessions per year for stage 4 CKD patients because it saves money - up to $12,000 per patient annually by delaying dialysis.
Apps like Kidney Kitchen (downloaded over 250,000 times) let you scan barcodes and track nutrients. New AI tools, being piloted at Mayo Clinic in 2024, sync with your lab results and adjust recommendations automatically. And if you have diabetes - which causes 44% of new CKD cases - you’re facing a double challenge. Heart-healthy foods for diabetics are often high in potassium or phosphorus. Your dietitian will help you find the overlap.
What’s Next? Personalized Renal Nutrition
The future of renal diets is personal. The NIH launched the PRIORITY study in January 2024 to see if genetic testing can predict how your body handles potassium and phosphorus. Early research suggests your gut microbiome may play a role too. Dr. Dominic Raj found that prebiotic fibers like inulin can reduce phosphorus absorption by 15-20%. And in September 2023, the FDA approved Keto-1 - the first medical food for CKD - designed to give essential amino acids without the phosphorus or potassium burden.
Some experts, like Dr. Sankar Navaneethan in JAMA Internal Medicine, argue that extreme restriction isn’t always better. He suggests focusing on food quality - choosing whole, unprocessed foods over ultra-processed ones - rather than obsessing over exact numbers. That’s a shift worth noting. You don’t need to be perfect. You need to be consistent. Small, smart changes add up.
Frequently Asked Questions
Can I still eat fruits and vegetables on a renal diet?
Yes, but you need to choose carefully and control portions. Low-potassium options include apples, berries, cabbage, cauliflower, and green beans. Leaching vegetables - soaking them in warm water for 2-4 hours, then boiling in plenty of water - can cut potassium by up to half. Avoid high-potassium choices like bananas, oranges, potatoes, tomatoes, and spinach unless they’re leached or eaten in very small amounts.
Is salt the only source of sodium I need to worry about?
No. Most sodium comes from processed foods - canned soups, frozen meals, deli meats, bread, cheese, and even some medications. Always check nutrition labels. One serving of canned soup can have more sodium than you’re allowed for the whole day. Look for "no salt added," "unsalted," or "low sodium" options, but still check the milligrams per serving.
Why are phosphorus additives worse than natural phosphorus?
Your body absorbs nearly all the phosphorus added to processed foods (90-100%), while it only absorbs about half of the phosphorus naturally found in meat, dairy, and legumes. Additives like phosphoric acid in colas and sodium phosphate in processed cheeses are designed to enhance flavor and shelf life - but they flood your system with phosphorus your kidneys can’t handle. Avoid colas, processed cheeses, and anything with "phos" in the ingredient list.
Do I need to limit protein on a renal diet?
Yes, but not too much. Too little protein can lead to muscle loss and malnutrition, especially in older adults. Current guidelines recommend 0.55-0.8 grams of high-quality protein per kilogram of body weight daily. Good sources include eggs, fish, chicken, and lean meats. Avoid plant proteins like beans and lentils if your phosphorus is high - they’re high in both protein and phosphorus.
Can I drink coffee or tea?
Yes, in moderation. One cup of coffee or tea is usually fine. But avoid adding milk or creamers - they’re high in phosphorus and potassium. Stick to water, lemon water, or herbal teas without added fruit flavors. If you’re on fluid restriction, count your coffee as part of your daily limit.
How long does it take to get used to a renal diet?
Most people need 3 to 6 months to adjust. The first few weeks are hardest - food tastes bland without salt, and giving up favorite fruits or drinks feels unfair. But your taste buds adapt. You start enjoying the natural flavors of food again. Working with a renal dietitian helps you make gradual changes instead of overwhelming yourself.



Comments
I swear I thought I was eating healthy until I read this. I was eating canned soup every day like it was a goddamn lifeline. Now I’m scared to open my pantry. My blood pressure dropped 8 points in two weeks just by swapping out the soup for homemade broth. Who knew my favorite comfort food was slowly killing me?
i just wanna say that i used to think potassium was bad because bananas are bad but then i learned that like half a cup of blueberries has less than a banana and now i eat them every morning with my oatmeal and i feel way better like my legs dont feel heavy anymore and my heart stops skipping so much i dont even know why people make this so hard its just about swapping things out not giving up food forever
This is the most practical renal guide I’ve ever seen. No fluff. Just facts. I’ve been on this diet for 8 months and it’s the first time I’ve felt like I actually have control. I started cooking more. Started reading labels. Even my kids are eating cleaner now. No more frozen pizza nights.
u think u know but u dont. in india we eat dal and roti every day and people think its healthy but dal is full of phos and roti is whole wheat so its worse than bread. i switched to white rice and boiled veggies and my creatinine dropped. no one told me this. doctors here dont even know.
To everyone saying this is too hard - I get it. I was there. But this isn’t about perfection. It’s about progress. I started by cutting out one thing a week. First it was soda. Then deli meat. Then canned beans. Now I cook almost everything from scratch. And yeah, it tastes different. But it tastes *mine*. You don’t have to be a chef. You just have to be consistent.
I’ve been doing this for 2 years. The biggest mistake I made was thinking I had to eat nothing but plain chicken and rice. Turns out, you can still have flavor. Garlic powder, lemon juice, vinegar, black pepper - they’re your new best friends. And yes, I still eat apples. Just not 5 a day.
I used to think the renal diet was just for old people. Then my dad got diagnosed and I saw how fast he lost muscle. We started tracking his protein intake and now he’s stronger than he’s been in years. This isn’t about dying slower. It’s about living better.
Let’s be real - this whole diet is a scam. The FDA approves phosphorus additives because Big Food doesn’t want you to know. And now they’re selling you "phosphate-binding rice" like it’s magic? Please. Just stop eating processed crap. That’s it. No fancy apps. No $200 supplements. Just real food. Stop paying for fear.
The scientific consensus remains clear: dietary phosphorus restriction in non-dialysis chronic kidney disease patients is associated with improved mineral metabolism and reduced vascular calcification risk, per KDOQI guidelines. While individual variation exists, adherence to evidence-based protocols remains clinically superior to anecdotal approaches. Dietary counseling should be standardized and insurer-reimbursed.
I keep thinking about how food used to be. Before additives. Before labels. Before we turned meals into chemistry experiments. Maybe the real problem isn’t that we’re eating too much phosphorus - it’s that we’ve forgotten what food actually is. My grandma cooked with salt, butter, and time. No "phos" in sight. Maybe we don’t need more rules. Maybe we just need to go back.
I’ve been on dialysis for 3 years. This diet kept me off it for 5. I’m not saying it’s easy. But it’s worth it. The first time I ate a lemon with my fish and didn’t feel like I was going to explode? That was freedom.