Why do so many people still think generic drugs don’t work as well?
It’s a simple question with a complicated answer. You walk into the pharmacy, pick up your prescription, and see a different name on the bottle. Instead of Lyrica, it says pregabalin. Instead of Viagra, you get sildenafil. You feel confused. Was this a mistake? Is this cheaper version safe? Will it even help?
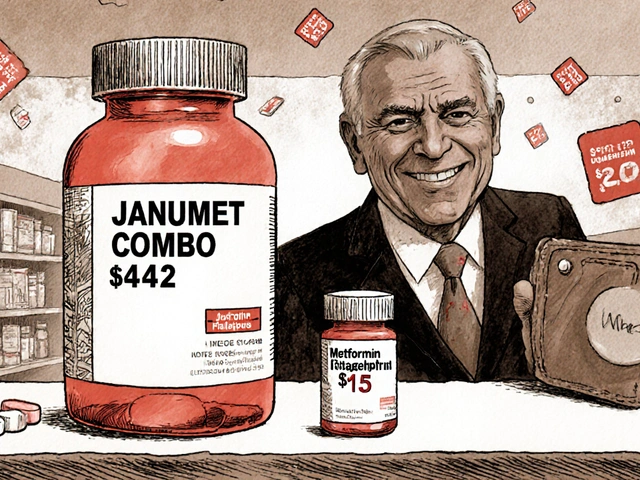
You’re not alone. In the U.S., 9 out of 10 prescriptions filled are for generic drugs. They’ve saved the healthcare system nearly $2 trillion over the last decade. But despite all that, nearly 4 in 10 Americans still believe generics are weaker, less safe, or not as effective as brand-name drugs. Why? Because the information they’re given is either too technical, too vague, or just plain misleading.
What exactly is a generic drug - and how is it really different?
A generic drug is not a copy. It’s not a knockoff. It’s the same medicine, made to meet the exact same standards as the brand-name version. The FDA requires that generics have the same active ingredient, same strength, same way of taking it (pill, liquid, injection), and same effect in the body.
Think of it like this: Tylenol and acetaminophen are the same thing. One is a brand name, the other is the medicine’s real name. Just like Kleenex is to tissues, or Band-Aid is to adhesive bandages - the brand is just one version of the product. The generic version has to prove it works the same way before it’s approved. That means it delivers the same amount of medicine into your bloodstream, within a very tight range - 80% to 125% of the brand-name drug. That’s not a guess. That’s science.
The differences you see? Color, shape, filler ingredients. Those don’t affect how the drug works. They’re just there to make the pill look different or easier to swallow. Some generics use lactose instead of sugar. Others use a different dye. None of that changes the medicine’s power.
How do language guides fix the confusion?
Consumer language guides are simple, clear tools made to turn confusing medical jargon into everyday talk. They’re not written for doctors. They’re written for people who just want to know: Will this work? Is it safe? Why is it cheaper?
Good guides use analogies people already understand. They compare generic drugs to store-brand cereal. You wouldn’t think store-brand cereal is less nutritious just because it doesn’t have a cartoon on the box. The same logic applies to medicine.
They also use visuals. Side-by-side pictures of a brand-name pill and its generic version. Labels that show the active ingredient in big, bold letters. Simple charts that say: Same medicine. Same dose. Same effect. Lower price.
The FDA’s Generic Drug Facts page, updated every quarter, is one of the best examples. It breaks down complex terms like “bioequivalence” into plain language. It answers the most common questions in under 500 words. And it’s backed by data - studies show patients who read these guides understand their meds 37% better than those who get standard pamphlets.
When generics aren’t exactly the same - and why that matters
But here’s the catch: not every drug is the same across all versions. Some medicines have what’s called a “narrow therapeutic index.” That means the difference between the right dose and a harmful one is very small. For these, even tiny changes in how the body absorbs the drug can matter.
Drugs like warfarin (for blood clots), levothyroxine (for thyroid), and phenytoin (for seizures) fall into this category. Some studies have shown that switching between different generic versions of these drugs can cause problems - not because the generic is bad, but because the body reacts differently to slight changes in how the pill breaks down.
That’s why the best language guides don’t say, “All generics are identical.” They say: “For most drugs, generics work just as well. For a few, your doctor may recommend sticking with one brand or generic version. Ask if yours is one of them.”
That small shift in wording makes all the difference. It doesn’t scare people. It empowers them.
What do pharmacists actually say when you ask about generics?
Most pharmacists now use the same three-point script when explaining generics:
- Same active ingredient. “This pill has the same medicine in it as the brand-name version.”
- Same effect. “It has to work the same way to get FDA approval. That means your body gets the same amount of medicine.”
- Same savings. “You’ll save an average of $387 per prescription - that’s hundreds of dollars a year.”
They spend about 90 seconds on this. Not five minutes. Not a lecture. Just clear, calm facts.
And it works. Patients who hear this are 22% more likely to stick with the generic. They’re 34% less likely to ask for the brand-name version again.

What’s new in 2026 - and what’s coming next
Things are changing fast. In early 2025, Medicare Part D plans were required to start giving out standardized patient education materials that meet federal health literacy standards. That means no more confusing brochures with tiny print and medical terms no one understands.
The FDA launched a $4.7 million initiative in 2023 to create custom guides for high-risk drugs like levothyroxine and digoxin. These aren’t one-size-fits-all. They’re tailored to the specific risks of each medicine.
And now, some pharmacies are testing AI tools that adjust the explanation based on how much a patient already knows. If you’re a retired teacher with a college degree, you get a slightly more detailed version. If you’re a single parent juggling three jobs and barely reading past the first sentence of a text, you get the simplest version - with pictures, big fonts, and no jargon.
What you can do today
You don’t need to wait for a guide to be handed to you. You can ask for one.
- When you get a generic prescription, ask: “Can you show me the difference between this and the brand-name version?”
- Look up the FDA’s Generic Drug Facts page. It’s free, updated regularly, and easy to read.
- If you’re on a drug like levothyroxine or warfarin, ask your doctor if you should stick with the same generic version every time.
- Don’t be afraid to say: “I’m not sure this is the same. Can you explain it again?”
Generic drugs aren’t a compromise. They’re a smart choice - if you understand them. And with the right information, there’s no reason to pay more for the same medicine.
Why this matters for your health - and your wallet
Every time someone chooses a generic over a brand-name drug, the system saves money. That money stays in people’s pockets. It keeps premiums lower. It helps more people afford their medicines.
But if people keep avoiding generics because they’re afraid, the savings disappear. In 2023, unnecessary brand-name prescriptions cost the system $3.2 billion. That’s $3.2 billion that could have gone to more people getting the care they need.
Understanding generics isn’t just about saving money. It’s about making sure you get the right treatment - without fear, confusion, or unnecessary cost.