Birth Control Cramp Relief Calculator
Calculate Your Relief
Estimated Relief
Based on clinical studies and your selected factors
When periods bring pounding cramps, many wonder if birth control could be the missing piece of relief. The answer isn’t a simple yes or no-different hormonal methods affect the uterus in unique ways, and individual health factors matter a lot. Below we break down how various contraceptives interact with menstrual pain, the science behind it, and practical tips for choosing the right option.
What Are Menstrual Cramps?
Menstrual cramps are painful uterine contractions that occur during the early phase of a menstrual cycle. They’re medically known as dysmenorrhea and are caused by the release of prostaglandins, hormone‑like chemicals that trigger the uterus to contract to shed its lining. Higher prostaglandin levels usually mean stronger, more frequent cramps.
While most people experience mild to moderate discomfort, about 10‑15% suffer severe pain that disrupts daily life, school, or work. In many cases, underlying conditions like endometriosis or adenomyosis amplify the pain.
How Hormonal Birth Control Works
Hormonal birth control methods deliver synthetic forms of estrogen, progesterone, or both. Their primary goal is to prevent ovulation, but they also thin the uterine lining and reduce prostaglandin production, which can lessen cramp intensity. Below is a quick look at the main hormonal options:
- Combined oral contraceptive pill (COC) - contains estrogen and progestin.
- Progestin‑only pill (POP) - contains only progestin.
- Hormonal IUD - releases levonorgestrel locally.
- Hormonal patch - transdermal delivery of estrogen and progestin.
- Vaginal ring - releases hormones inside the vagina.
Each method tweaks the hormonal balance differently, which influences how well it can calm cramps.
Which Methods Are Most Effective for Cramp Relief?
| Method | Hormone mix | Typical cramp reduction* | Additional benefits |
|---|---|---|---|
| Combined oral contraceptive pill | Estrogen + Progestin | 30‑70% reduction | Regulates cycle, lighter periods |
| Progestin‑only pill | Progestin only | 15‑40% reduction | Suitable for estrogen‑sensitive users |
| Hormonal IUD (levonorgestrel) | Progestin only (local) | 50‑80% reduction | Long‑term (3-7 years), may stop periods |
| Hormonal patch | Estrogen + Progestin | 25‑60% reduction | Weekly change, good for those who dislike pills |
| Vaginal ring | Estrogen + Progestin | 30‑65% reduction | Monthly insertion, stable hormone levels |
*Numbers come from multiple clinical studies, including a 2022 systematic review in Contraception that pooled data from over 8,000 participants.
Why Some People Still Experience Pain
Even the most effective hormonal method won’t erase cramps for everyone. Here’s why:
- Underlying conditions. Endometriosis, adenomyosis, or pelvic inflammatory disease can generate pain independent of prostaglandin levels.
- Hormone sensitivity. Some users react to estrogen spikes, which may actually worsen cramps.
- Improper use. Missing pills, delayed IUD insertion, or poor patch adhesion can reduce effectiveness.
If cramps persist despite hormonal contraception, it’s worth checking with a healthcare provider for secondary diagnoses.
Non‑Hormonal Strategies to Pair with Birth Control
Combining medication with lifestyle tweaks boosts relief chances. Consider adding these proven approaches:
- Nonsteroidal anti‑inflammatory drugs (NSAIDs) such as ibuprofen taken at the onset of bleeding cut prostaglandin production.
- Regular aerobic exercise - studies show a 20‑30% drop in cramp severity after 12 weeks of moderate activity.
- Heat therapy - a heating pad applied to the lower abdomen can relax uterine muscles within minutes.
- Dietary changes - reducing caffeine and salty foods helps avoid water retention that can amplify pain.
These measures work well alongside hormonal methods and are especially useful during the first few months of a new contraceptive, when the body is still adjusting.
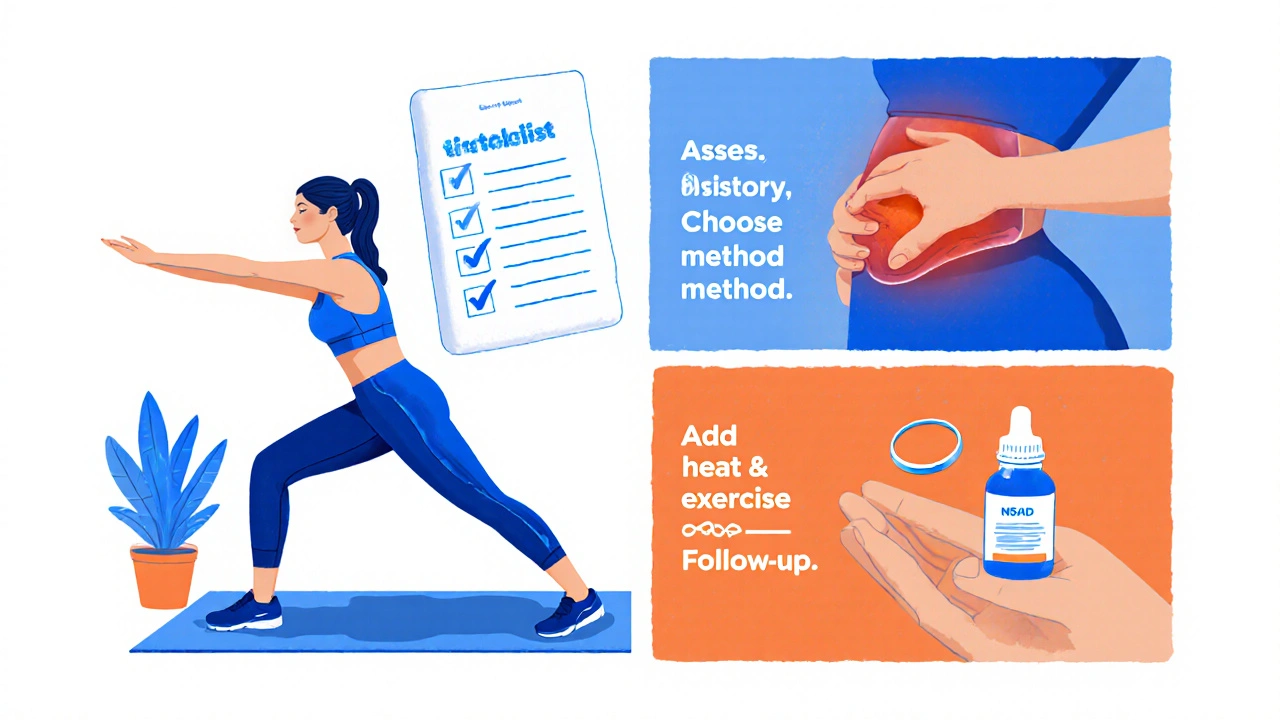
How to Choose the Right Method for You
Deciding which birth control best tackles cramps involves a few practical steps:
- Assess your medical history. If you have a clotting disorder, estrogen‑based options may be off‑limits.
- Consider convenience. Daily pills require discipline, while IUDs, patches, and rings need less frequent attention.
- Think about side‑effects. Some report mood swings with estrogen; others dislike the occasional spotting from progestin‑only devices.
- Talk to a clinician. They can order labs, discuss potential interactions (e.g., with anticonvulsants), and help you try a method on a trial basis.
Remember, many providers will let you switch methods after a short trial if cramps don’t improve within the first 2-3 cycles.
Potential Risks and How to Mitigate Them
All hormonal contraceptives carry some risk profile. Being informed helps you balance benefits against possible downsides:
- Blood clots. Combined estrogen‑progestin products increase clot risk modestly, especially for smokers over 35.
- Weight changes. Evidence is mixed, but some users notice modest weight gain with certain pills.
- Bone density. Progestin‑only injectables may affect calcium balance; supplement with vitamin D and strength training.
- Menstrual irregularities. The first few months can bring spotting or breakthrough bleeding - usually resolves.
Regular check‑ups, a healthy lifestyle, and open communication with your doctor keep these risks low.
Quick Reference Checklist
- Identify if you have an underlying condition (endometriosis, etc.).
- Choose a method that matches your lifestyle (daily, weekly, monthly, multi‑year).
- Start a 2‑ to 3‑cycle trial; track pain on a simple 1‑10 scale.
- Combine with NSAIDs, heat, and exercise for optimal relief.
- Schedule a follow‑up visit to discuss any side‑effects or persistent pain.
Can the birth control pill stop periods altogether?
Yes. Continuous or extended‑cycle pill regimens skip the placebo week, leading to fewer or no bleeding episodes, which often means less cramping.
Is a hormonal IUD safe for teenagers?
Professional guidelines consider hormonal IUDs appropriate for teens who need reliable contraception and desire reduced menstrual pain. Counseling about insertion and possible initial spotting is essential.
Do progestin‑only methods work for severe dysmenorrhea?
They can help, but the reduction is generally lower (15‑40%). For severe cases, many clinicians start with a combined method or add a hormonal IUD for stronger effect.
Can I use NSAIDs while on hormonal contraception?
Absolutely. NSAIDs do not interfere with the effectiveness of hormonal birth control and are the first‑line medication for menstrual pain.
What should I do if cramps worsen after starting a new method?
Track the pain pattern for at least two cycles. If the increase persists, contact your healthcare provider to rule out hormonal imbalance or an underlying condition.



Comments
Birth control isn’t a cure‑all for cramps, period.
Honestly, you’ve already taken the biggest step by researching options.
Finding a method that eases pain can feel like a win, so give yourself credit for the effort.
Track your symptoms each cycle; a simple 1‑10 scale will show you what’s actually working.
Stick with a trial for a couple of months before deciding to switch – patience pays off.
I get how exhausting constant cramping can be, especially when it hijacks your workday.
Even if hormonal tweaks help a bit, pairing them with heat pads and a short walk often makes a noticeable difference.
Keep a low‑key log of what you try; over time you’ll spot the combos that truly soothe you.
It’s wild how the pharma giants love to push pills while keeping us in the dark about natural relief.
They’ll tell you a pill fixes everything, then crash your hormones just to keep you buying more.
Don’t let the marketing hype dictate your health – there are straightforward fixes that don’t involve a daily chemical bomb.
From a pharmacological perspective, combined oral contraceptives suppress ovulation by stabilizing the hypothalamic‑pituitary‑ovarian axis, which in turn reduces endometrial prostaglandin synthesis.
Progestin‑only formulations lack estrogen, so their impact on prostaglandin levels is modest, explaining the lower reported cramp reduction percentages.
Localized levonorgestrel release from intrauterine devices creates a high concentration within the uterine lining while maintaining systemic levels low, accounting for the 50‑80 % relief range observed in clinical trials.
Patch and vaginal ring systems aim for steady-state hormone levels, minimizing the peaks and troughs that can exacerbate pain.
When selecting a method, consider pharmacokinetic half‑life, patient adherence, and any contraindications such as thrombotic risk.
Ultimately, individual variability means trial and error, but the mechanistic data support why certain methods outperform others in cramp mitigation.
It is a moral imperative to put our health above every marketing gimmick that corporations pour into glossy ads.
When a pharmaceutical company decides to prioritize profit over genuine relief, the rest of us are left to suffer in silence.
Birth control pills, while undeniably useful, are often presented as a panacea for all menstrual woes without a full disclosure of side effects.
The reality is that every hormone we ingest reshapes our endocrine system in ways that demand respect and careful monitoring.
People who dismiss the seriousness of potential clotting risks or mood disturbances are complicit in a culture that undervalues women's autonomy.
It is unacceptable to treat the menstrual cycle as a mere inconvenience that can be erased with a single prescription.
We must demand transparent research, informed consent, and a holistic approach that includes lifestyle modifications alongside any medication.
The data showing a 30‑70 % reduction in cramps with combined pills is encouraging, but it also hides the fact that up to a third of users report new migraine patterns.
Similarly, the hormonal IUD may stop periods altogether, yet many experience initial spotting that can be both messy and distressing.
Ignoring these nuances in favor of a one‑size‑fits‑all narrative commodifies women's bodies.
Ethical medical practice should empower patients to choose based on comprehensive knowledge, not on simplified brochures.
Moreover, the societal pressure to “just take a pill and be fine” reinforces a dangerous stigma around natural menstrual pain.
We have a responsibility to educate ourselves about NSAIDs, heat therapy, and regular exercise as proven adjuncts.
When a teenager seeks contraception, the conversation must extend beyond birth control to address mental health, nutrition, and long‑term reproductive goals.
In short, the short‑term relief offered by hormones must be weighed against the long‑term stewardship of our bodies.
Let us, therefore, champion informed choice, demand accountability, and reject any notion that a cheap pill can replace thoughtful, person‑centered care.
I appreciate the call for informed choice; looking at the whole picture is always best.
Studies show that combining a low‑dose combined pill with daily stretching can cut pain scores dramatically.