When your liver is damaged over years-by alcohol, fatty liver, hepatitis, or other causes-it doesn’t just heal. It scars. That scarring is cirrhosis, the final stage of chronic liver disease. It’s not a single event. It’s a slow, silent breakdown that turns healthy tissue into stiff, tangled scar tissue. By the time symptoms show up, the damage is often advanced. But knowing what to watch for and how to act can change everything.
What Cirrhosis Really Does to Your Body
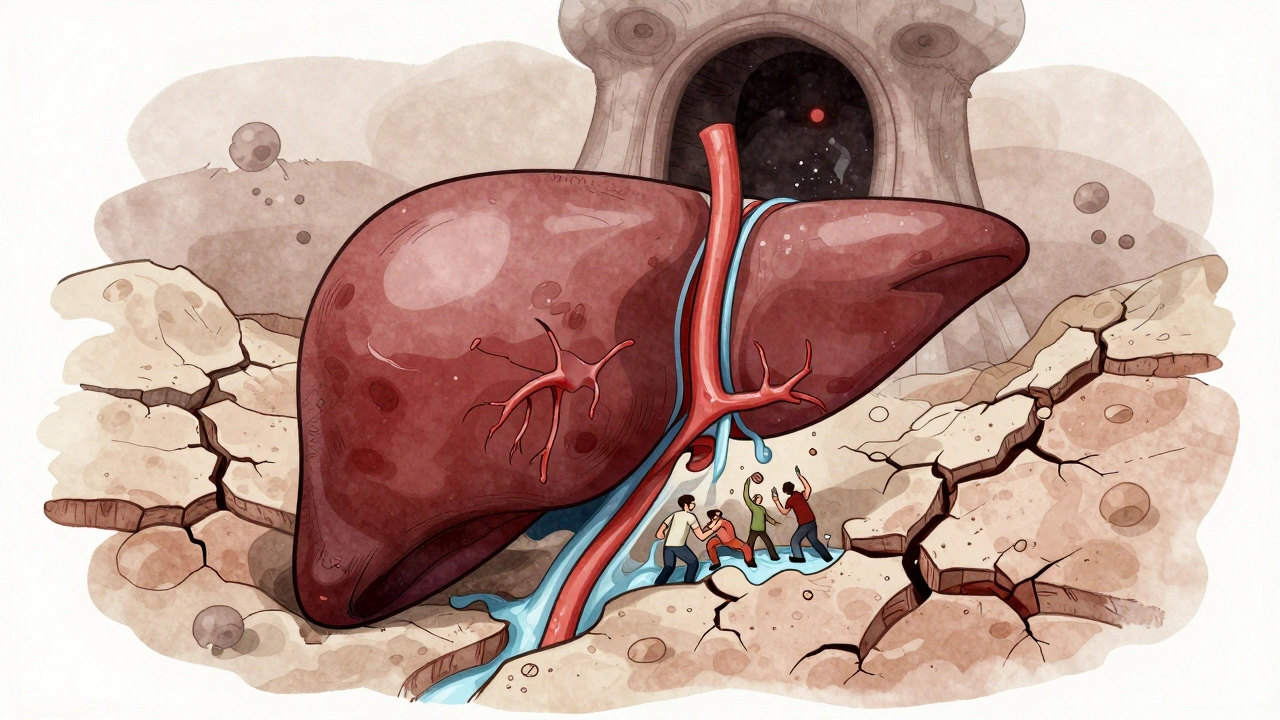
The liver doesn’t just filter toxins. It makes proteins, stores energy, cleans your blood, and helps digest food. When cirrhosis sets in, all of that slows down. Blood can’t flow through the liver easily because of the scar tissue. That creates pressure in the portal vein-the main blood vessel bringing blood from your gut to your liver. This is called portal hypertension, and it’s the root of most serious complications. You might not feel anything at first. Many people have compensated cirrhosis-their liver is scarred, but still doing enough to keep them feeling okay. That’s when the real danger hides. Without regular monitoring, it can suddenly shift into decompensated cirrhosis, where the liver can’t keep up anymore. That’s when life-threatening problems start.The Big Five Complications
There are five major complications that define decompensated cirrhosis. Each one has clear signs, measurable risks, and proven ways to manage them.- Ascites: Fluid builds up in your belly. It’s not just swelling-it’s a sign your liver is failing to make albumin, a protein that keeps fluid in your blood vessels. About half of people with cirrhosis develop ascites within 10 years. You might notice your pants getting tight, your belly feeling heavy, or even trouble breathing when lying down.
- Variceal bleeding: High pressure in the portal vein forces blood to find new paths. It bulges veins in your esophagus or stomach. These are called varices. They’re thin-walled and can rupture without warning. Bleeding from them is sudden, dangerous, and kills 15-20% of people during the first episode.
- Hepatic encephalopathy: Your liver can’t remove ammonia from your blood. That toxin builds up and affects your brain. You might feel confused, forgetful, or sluggish. Some people sleep more than usual. Others become irritable or even hallucinate. It’s often called "brain fog," but it’s a medical emergency.
- Spontaneous bacterial peritonitis (SBP): The fluid in your belly can get infected-even without an open wound. This infection happens without any obvious source, and it’s deadly if missed. Up to 30% of people with ascites develop SBP, and 20-40% of those cases end in death during hospitalization.
- Hepatocellular carcinoma (HCC): Cirrhosis turns your liver into a breeding ground for cancer. About 2-8% of people with cirrhosis develop liver cancer each year. It grows fast, but if caught early through regular scans, it’s treatable.
How Doctors Measure How Bad It Is
Not all cirrhosis is the same. Two people with the same diagnosis can have very different outcomes. That’s why doctors use scores to predict risk. The Child-Pugh score looks at five things: bilirubin, albumin, INR (a blood clotting test), ascites, and encephalopathy. It gives you a class: A, B, or C. Class A means you’re doing well-100% survive a year. Class C? Only 45% make it past 12 months. Even more precise is the MELD score (Model for End-Stage Liver Disease). It uses three blood tests: bilirubin, creatinine (kidney function), and INR. A score under 10 means low risk. A score over 15 means you’re in serious danger. Over 20? You’re likely on the transplant list. A score above 30 means you have a 70% chance of dying within a year without a transplant. These scores aren’t just numbers. They decide who gets a liver first. And they guide whether you need daily meds, frequent scans, or hospital visits.Managing the Complications-Step by Step
There’s no cure for cirrhosis yet. But we can stop it from getting worse-and prevent the worst complications.- For ascites: The first step is cutting salt to under 2 grams a day. That’s harder than it sounds-processed foods, bread, sauces are all loaded. Then come diuretics: spironolactone (100 mg daily) and sometimes furosemide. Most people respond well. But if fluid keeps coming back, you’ll need a procedure called paracentesis-where doctors drain the fluid with a needle. To prevent shock after draining, you get albumin IV. This cuts complications from 37% down to 10%.
- For varices: If you have large varices, you’ll be put on a beta-blocker like propranolol or nadolol. These lower pressure in the portal vein and cut bleeding risk by nearly half. If you’ve bled before, you’ll also get banding during an endoscopy-tiny rubber bands placed around the veins to stop them from bursting. You’ll need repeat endoscopies every 1-2 years.
- For hepatic encephalopathy: Lactulose is the go-to. It’s a syrup that pulls ammonia out of your gut and into your stool. You take it 2-3 times a day until you have 2-3 soft bowel movements daily. If that’s not enough, rifaximin (an antibiotic that doesn’t get absorbed) is added. It cuts hospital readmissions by 58%.
- For SBP: If you have ascites, you’ll likely be on a daily antibiotic like norfloxacin or ciprofloxacin to prevent infection. If you get sick with fever or belly pain, you go straight to the hospital. Antibiotics start immediately.
- For liver cancer: Every six months, you get an ultrasound. Sometimes a CT or MRI is added. This isn’t optional-it’s life-saving. Early tumors (under 2 cm) can be removed or burned off. Late ones? Often not treatable.
What’s New in Treatment
The last few years have brought real hope. In March 2024, the FDA approved resmetirom (Rezdiffra) for people with MASH (formerly called NASH) and cirrhosis. In trials, it reduced liver scarring in over 20% of patients after a year. This is the first drug approved to directly target liver fibrosis in cirrhosis. Artificial intelligence is stepping in too. A tool called CirrhoPredict uses routine blood tests to forecast who’s likely to decompensate in the next 90 days. It’s 88% accurate. That means doctors can act before you get sick-adjusting meds, scheduling scans, or even moving you up the transplant list. And liver transplant allocation changed in February 2024. Instead of just using MELD scores, centers now also consider quality of life. Someone with frequent brain fog, even if their MELD is low, can now get priority. This recognizes that cirrhosis isn’t just about survival-it’s about living.
Life With Cirrhosis-The Human Side
Numbers matter. But so do lived experiences. People with cirrhosis often describe exhaustion that no amount of sleep fixes. One survey found 78% of patients had fatigue severe enough to stop working or doing daily tasks. Lactulose helps encephalopathy-but it causes constant diarrhea. One Reddit user said it made him miss 12 family events this year. Paracentesis can be painful. Over 70% of patients rate the pain as 5 or higher on a 10-point scale. And waiting for a transplant? The odds are stacked. In 2022, there were 11,346 people on the list in the U.S. and only 8,391 transplants performed. Twelve percent of people die waiting. But there’s also hope. One patient wrote: "18 months after transplant, my MELD score dropped from 28 to 9. I went back to full-time work." That’s the goal: not just surviving, but living.What You Can Do Right Now
If you have cirrhosis:- Get your liver checked every 3-6 months. Don’t skip appointments.
- Take every pill exactly as prescribed-even if you feel fine.
- Avoid alcohol completely. Even one drink can trigger rapid decline.
- Get vaccinated for hepatitis A, hepatitis B, flu, and pneumonia.
- Track your weight daily. A 2-pound gain in 24 hours could mean fluid buildup.
- Ask for a referral to a dietitian. A 2g sodium diet is hard to do alone.
- Ask about transplant evaluation. Don’t wait until you’re in crisis.
Final Thought
Cirrhosis is not a death sentence. But it’s not something you can ignore. It demands structure: regular monitoring, strict medication, and lifestyle changes. The good news? We have more tools than ever to slow it, manage it, and sometimes even reverse early damage. The key is acting early-before the complications start.Can cirrhosis be reversed?
In early stages, yes-sometimes. If you stop drinking, lose weight, or cure hepatitis C, your liver can repair some of the damage. Studies show fibrosis can improve in up to 40% of patients with early cirrhosis if the cause is removed. But once extensive scarring and nodules form, the structure is permanent. The goal then shifts to preventing further damage and complications.
How do I know if I have portal hypertension?
You won’t feel it directly. But its effects show up as ascites, varices, or an enlarged spleen. Doctors measure it with a special test called HVPG (hepatic venous pressure gradient), done during a liver catheterization. If you have ascites or varices, you likely have portal hypertension-even if it’s never been measured.
Is a liver transplant the only option for advanced cirrhosis?
It’s the only cure. But not everyone needs it right away. Many people live for years with well-managed cirrhosis. Transplant is considered when MELD score is high (usually over 15), when complications can’t be controlled, or when liver cancer develops. You don’t need to be dying to be evaluated-early referral improves outcomes.
Can I still work with cirrhosis?
Many people do-especially in compensated stages. But fatigue and brain fog make some jobs impossible. If you’re on diuretics, you’ll need bathroom access. If you’re on lactulose, you’ll need to plan around frequent bowel movements. Talk to your doctor about accommodations. Some people switch to remote work or part-time roles. Disability benefits are available if you can’t work.
What happens if I miss a dose of my cirrhosis meds?
Missing a beta-blocker can raise your risk of bleeding. Skipping lactulose can trigger brain fog or confusion. Missing diuretics can cause fluid to build up fast. It’s not about one missed pill-it’s about consistency. Set phone alarms. Use pill organizers. Ask a family member to check in. Your liver can’t afford mistakes.
Why do I need an ultrasound every six months?
Liver cancer grows fast and often has no symptoms until it’s advanced. Ultrasound catches tumors early-when they’re small and treatable. In people who get screened, 70% of cancers are found at the earliest stage (BCLC 0/A). Without screening, only 30% are caught early. That difference means you can live years longer.
Does being overweight make cirrhosis worse?
Yes-especially if you have MASH (metabolic dysfunction-associated steatohepatitis). Fat in the liver causes inflammation, which speeds up scarring. Losing 7-10% of your body weight can reduce liver fat and inflammation. Even small weight loss helps. You don’t need to be thin-just healthier.
Can I drink alcohol if I have cirrhosis?
Absolutely not. Even one drink can trigger rapid liver damage, bleeding, or infection. Alcohol is the #1 cause of cirrhosis in Europe and a major cause in the U.S. If you’ve already developed cirrhosis, your liver has zero tolerance. Complete abstinence is non-negotiable.
How much sodium is too much?
Less than 2,000 mg per day. That’s about half a teaspoon of salt. But most of it comes from hidden sources: canned soups, bread, deli meats, soy sauce, salad dressings. Read labels. Cook at home. Avoid processed food. A dietitian can help you plan meals that taste good but stay under the limit.
What’s the difference between MELD and Child-Pugh?
Both measure liver failure, but MELD is more accurate for predicting short-term death and is used to prioritize transplant candidates. Child-Pugh is simpler and still used to classify overall severity. MELD uses only blood tests (bilirubin, creatinine, INR). Child-Pugh adds clinical signs like ascites and encephalopathy. Most centers use MELD for transplant decisions.
Managing cirrhosis isn’t about perfection. It’s about consistency. Every pill taken. Every appointment kept. Every salt shaker left on the counter. These small choices add up to years of life-and the chance to be there for the people who matter most.

Comments
Really well put together. I’ve been managing cirrhosis for 5 years now and this is the first time I’ve seen everything laid out so clearly. The part about lactulose causing constant diarrhea? Yeah, that’s real. I missed my niece’s wedding because I was stuck near a bathroom. But I’m alive, and that counts.
Keep pushing for regular scans. Early detection saved my life.
Also, if you’re on diuretics, drink water like it’s your job. Dehydration is sneaky.
Why do we even bother? The liver’s just gonna fail anyway. I saw my uncle die waiting for a transplant. All these meds and scans? Just money grabbers.
Alcohol’s fine in moderation. One beer ain’t gonna kill you.
Here we go again with the medical propaganda. They told you cirrhosis is from alcohol but what about the glyphosate in your bread and the fluoride in your water? The FDA approved resmetirom? That’s just phase 2 data cherry-picked by Big Pharma to sell more pills. Real healing comes from liver cleanses, apple cider vinegar, and sunlight. You think a pill fixes fibrosis? Wake up.
They don’t want you to know that the liver regenerates naturally if you stop eating processed crap. That’s why they push diuretics and transplants-profit. Your MELD score is a trap. You’re being manipulated into believing you need a transplant when all you need is to stop trusting doctors who get paid per procedure.
And don’t even get me started on the sodium thing. Salt isn’t the enemy. It’s the refined carbs and industrial seed oils that are poisoning you. Your ascites? It’s inflammation from gluten and soy. Cut those and you’ll see results. No drugs needed. No needles. Just common sense.
They’re scared of natural healing because it can’t be patented. The truth is buried under layers of medical jargon and insurance bureaucracy. You’re not sick-you’re being sold a system. Question everything. Even this post.
And if you’re still drinking coffee? You’re part of the problem. Switch to dandelion root tea. It’s nature’s diuretic. And it doesn’t come with a prescription label.
i read this whole thing and cried a little. i have cirrhosis from hcv and i’ve been on lactulose for 2 years. the diarrhea sucks but i dont miss my grandkids’ birthdays anymore. i set alarms for my meds and my wife checks on me. its hard but worth it.
also, i lost 12 lbs and my doctor said my liver enzymes improved. small wins matter. thank you for writing this.
ps. i typoed. sorry. my hands shake sometimes.
STOP listening to the naysayers. You can beat this. I was Class B Child-Pugh last year. Now I’m Class A. I quit sugar, started walking 30 minutes a day, and took every pill like it was my last chance. It’s not about being perfect-it’s about showing up. Every. Single. Day.
You’re not broken. You’re becoming stronger. And if you’re reading this? You’re already winning.
Good breakdown. I’m a nurse in Atlanta and I see this every week. The biggest mistake people make? Waiting until they’re dizzy or bloated to call their doctor. By then, it’s often too late for simple fixes.
Also-don’t ignore the mental health side. Depression hits hard with chronic illness. Therapy isn’t optional. It’s part of the treatment plan.
And yes, one beer is one too many. I’ve seen it kill people faster than the disease itself.
Excellent summary. As a hepatology nurse from India, I can confirm that early screening saves lives. In rural areas, patients often present only when ascites or bleeding occurs. Education is the missing link.
Resmetirom is promising but access remains limited outside the US. We need affordable generics.
Thank you for highlighting quality of life. It is not just about survival.
🙏
Let’s be honest: most of these patients are obese, alcoholic, or both. Why should society fund their transplants when they refused to change? The MELD score doesn’t account for personal responsibility. You made your bed. Now lie in it.
And lactulose? That’s just a fancy laxative. If you can’t handle diarrhea, maybe you shouldn’t have ruined your liver.
Also, why are we giving them dietitians? They’ll just eat junk anyway. It’s a waste of resources.
OMG this is SO important!! 🤯 I’ve been waiting for someone to explain this without jargon!! 💖 I just got diagnosed and I’m terrified but also… kinda empowered?? 🙌 I’m going to start tracking my weight and cut salt TODAY!! 🥑🚫
Also, I cried reading about the transplant waitlist. 12% die waiting?? That’s a national crisis. We need to fix this. 🏥💔
PS: I’m going to buy a pill organizer and name it ‘Liver Warrior’ 😎✨
Who gave you permission to write this? You sound like you’ve never met someone with cirrhosis. Did you even talk to a patient? Or are you just quoting guidelines you read in a journal? You talk about ‘small choices’ like they’re magic. What about the person who lost their job and can’t afford the diuretics? Or the one who lives alone and forgets because of brain fog? You don’t get to preach consistency when you’ve never lived it.
And what’s with the ‘transplant priority for brain fog’? So now we’re giving livers to people who can’t remember their kid’s birthday? What about the 70-year-old who’s been sober for 20 years and still waits? You’re not helping. You’re performing compassion.
Real people aren’t statistics. And you’re treating them like case studies.
Hey, I just wanted to say thank you for writing this. My dad has cirrhosis, and I’ve been trying to understand what he’s going through. This helped me more than three doctor visits.
I’m going to start helping him track his sodium and set up his pill organizer. He doesn’t like talking about it, but now I know what to ask.
And yes-he’s quit alcohol. No more beer on Sundays. It’s hard for him, but he’s trying. We’re all trying.
You’re not just sharing info. You’re giving people hope.
Thank you.