When a life-saving drug runs out, who gets it? This isn’t science fiction. In 2023, hospitals across the U.S. faced medication rationing for critical cancer drugs like carboplatin and cisplatin. Some patients waited weeks. Others got nothing. And the doctors making those calls? Many had no official guidelines. No training. No support. Just guilt, exhaustion, and impossible choices.
Why Medication Rationing Happens
Drug shortages aren’t rare anymore. They’re routine. The FDA tracked 319 active shortages in October 2023-up from just 61 in 2005. Most of these are sterile injectables: chemotherapy drugs, antibiotics, anesthetics. Why? A few big manufacturers control 80% of the market. If one factory has a quality issue, or a raw material shipment gets delayed, entire supply chains break. And when that happens, hospitals don’t get more drugs. They get less. And patients pay the price.What Ethical Rationing Actually Means
Rationing isn’t about picking favorites. It’s not about who has the loudest family or who’s the nicest nurse. Ethical rationing means using clear, fair rules to decide who gets treatment when there’s not enough to go around. The goal? To stop random, emotional, or biased decisions. To protect patients. To protect clinicians from being forced into moral nightmares. One widely accepted model is called Accountability for Reasonableness. It’s not fancy, but it works. It says: if you’re going to deny someone a drug, you must be able to explain why-publicly, clearly, and fairly. Four rules apply:- Publicity: Everyone should know how decisions are made.
- Relevance: Reasons must be based on medical evidence-not personal opinions.
- Appeals: Patients or families must be able to challenge a decision.
- Enforcement: Someone must make sure the rules are followed.
Who Decides? The Committee Model
The worst thing you can do is let one doctor decide alone. That’s bedside rationing. And it happens a lot. In fact, over half of all rationing decisions in U.S. hospitals are made by individual clinicians-no input, no review, no accountability. That leads to chaos. One hospital gives a drug to a 65-year-old. Another gives it to a 35-year-old. No one knows why. Better systems use multi-disciplinary committees. These teams include pharmacists, nurses, doctors, social workers, patient advocates, and ethicists. They meet. They review cases. They use data. They follow written criteria. A 2022 study in JAMA Internal Medicine found hospitals with these committees had 32% fewer disparities in who got treatment. That’s not small. That’s life-changing. But here’s the problem: only 36% of U.S. hospitals have standing committees. And only 2.8% include an ethicist. Most are underfunded, understaffed, and overwhelmed. When a shortage hits, they scramble. It takes 14 to 72 hours just to get the committee together. In acute care, that’s too long.
How Do You Choose Who Gets the Drug?
There’s no perfect answer. But experts agree on five key criteria:- Urgency of need: Is the patient’s condition life-threatening right now?
- Chance of benefit: Will the drug actually help? Is there evidence?
- Duration of benefit: Will it extend life for months-or just weeks?
- Years of life saved: Does one patient have more potential years ahead?
- Instrumental value: Should healthcare workers or first responders get priority? (This one is controversial.)
The Real Problem: Inequality
Here’s the ugly truth: rationing doesn’t just happen in big hospitals. It hits rural clinics hardest. Sixty-eight percent of rural hospitals have no formal rationing plan. That means patients in small towns are more likely to get skipped. They’re also less likely to be told what’s happening. Only 36% of patients are informed about rationing decisions. That’s not transparency. That’s silence. And it’s worse for marginalized groups. A 2021 report found 78% of rationing protocols don’t include any equity checks. No data on race, income, insurance status, or zip code. So if a Black patient or a low-income patient gets left out, no one notices. No one questions it. That’s not just unfair. It’s dangerous.What Hospitals Are Doing Right
Some places are getting it right. The Minnesota Department of Health created a clear, step-by-step plan for carboplatin and cisplatin shortages. Tier 1: patients with curative intent and no alternatives. Tier 2: patients with high survival potential. Tier 3: palliative care. No guessing. No favoritism. Hospitals that use this system also track every decision in their electronic records. They log: why the drug was given, who decided, and whether the patient was told. Only 22% of hospitals do this. But those that do see less burnout. Less guilt. Less conflict. One Mayo Clinic study found hospitals with ethics-involved committees had 41% lower clinician distress scores. That matters. When doctors are traumatized, care suffers.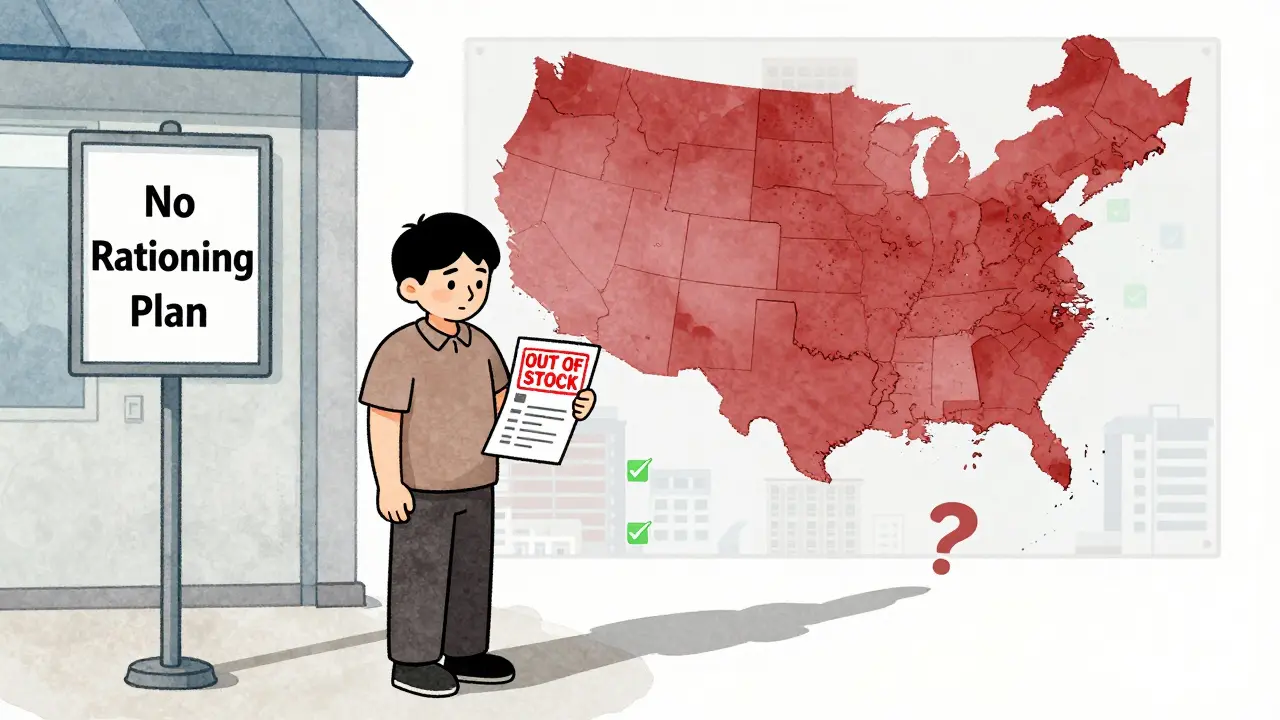
What Patients and Families Should Know
If you or a loved one is facing a drug shortage, ask these questions:- Is there a formal rationing plan in place?
- Who made the decision about my treatment?
- Can I see the criteria they used?
- Can I appeal if I disagree?
- Was I told why I’m not getting the drug?