When a life-saving drug runs out, who gets it? This isn’t science fiction. In 2023, hospitals across the U.S. faced medication rationing for critical cancer drugs like carboplatin and cisplatin. Some patients waited weeks. Others got nothing. And the doctors making those calls? Many had no official guidelines. No training. No support. Just guilt, exhaustion, and impossible choices.
Why Medication Rationing Happens
Drug shortages aren’t rare anymore. They’re routine. The FDA tracked 319 active shortages in October 2023-up from just 61 in 2005. Most of these are sterile injectables: chemotherapy drugs, antibiotics, anesthetics. Why? A few big manufacturers control 80% of the market. If one factory has a quality issue, or a raw material shipment gets delayed, entire supply chains break. And when that happens, hospitals don’t get more drugs. They get less. And patients pay the price.What Ethical Rationing Actually Means
Rationing isn’t about picking favorites. It’s not about who has the loudest family or who’s the nicest nurse. Ethical rationing means using clear, fair rules to decide who gets treatment when there’s not enough to go around. The goal? To stop random, emotional, or biased decisions. To protect patients. To protect clinicians from being forced into moral nightmares. One widely accepted model is called Accountability for Reasonableness. It’s not fancy, but it works. It says: if you’re going to deny someone a drug, you must be able to explain why-publicly, clearly, and fairly. Four rules apply:- Publicity: Everyone should know how decisions are made.
- Relevance: Reasons must be based on medical evidence-not personal opinions.
- Appeals: Patients or families must be able to challenge a decision.
- Enforcement: Someone must make sure the rules are followed.
Who Decides? The Committee Model
The worst thing you can do is let one doctor decide alone. That’s bedside rationing. And it happens a lot. In fact, over half of all rationing decisions in U.S. hospitals are made by individual clinicians-no input, no review, no accountability. That leads to chaos. One hospital gives a drug to a 65-year-old. Another gives it to a 35-year-old. No one knows why. Better systems use multi-disciplinary committees. These teams include pharmacists, nurses, doctors, social workers, patient advocates, and ethicists. They meet. They review cases. They use data. They follow written criteria. A 2022 study in JAMA Internal Medicine found hospitals with these committees had 32% fewer disparities in who got treatment. That’s not small. That’s life-changing. But here’s the problem: only 36% of U.S. hospitals have standing committees. And only 2.8% include an ethicist. Most are underfunded, understaffed, and overwhelmed. When a shortage hits, they scramble. It takes 14 to 72 hours just to get the committee together. In acute care, that’s too long.
How Do You Choose Who Gets the Drug?
There’s no perfect answer. But experts agree on five key criteria:- Urgency of need: Is the patient’s condition life-threatening right now?
- Chance of benefit: Will the drug actually help? Is there evidence?
- Duration of benefit: Will it extend life for months-or just weeks?
- Years of life saved: Does one patient have more potential years ahead?
- Instrumental value: Should healthcare workers or first responders get priority? (This one is controversial.)
The Real Problem: Inequality
Here’s the ugly truth: rationing doesn’t just happen in big hospitals. It hits rural clinics hardest. Sixty-eight percent of rural hospitals have no formal rationing plan. That means patients in small towns are more likely to get skipped. They’re also less likely to be told what’s happening. Only 36% of patients are informed about rationing decisions. That’s not transparency. That’s silence. And it’s worse for marginalized groups. A 2021 report found 78% of rationing protocols don’t include any equity checks. No data on race, income, insurance status, or zip code. So if a Black patient or a low-income patient gets left out, no one notices. No one questions it. That’s not just unfair. It’s dangerous.What Hospitals Are Doing Right
Some places are getting it right. The Minnesota Department of Health created a clear, step-by-step plan for carboplatin and cisplatin shortages. Tier 1: patients with curative intent and no alternatives. Tier 2: patients with high survival potential. Tier 3: palliative care. No guessing. No favoritism. Hospitals that use this system also track every decision in their electronic records. They log: why the drug was given, who decided, and whether the patient was told. Only 22% of hospitals do this. But those that do see less burnout. Less guilt. Less conflict. One Mayo Clinic study found hospitals with ethics-involved committees had 41% lower clinician distress scores. That matters. When doctors are traumatized, care suffers.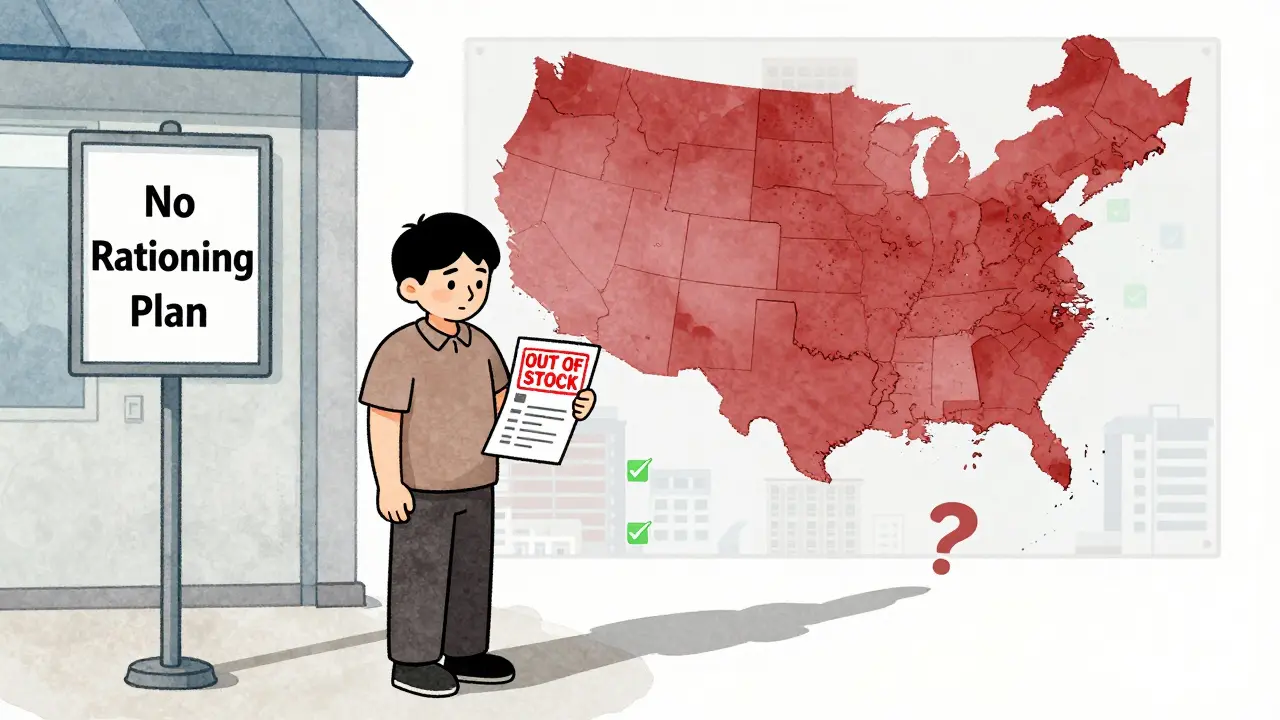
What Patients and Families Should Know
If you or a loved one is facing a drug shortage, ask these questions:- Is there a formal rationing plan in place?
- Who made the decision about my treatment?
- Can I see the criteria they used?
- Can I appeal if I disagree?
- Was I told why I’m not getting the drug?


Comments
This is the kind of systemic failure that keeps me up at night. No one should have to beg for a life-saving drug like it’s a favor.
Doctors shouldn’t be forced into god mode just because Big Pharma can’t make enough pills. This isn’t healthcare, it’s a corporate hostage situation.
The Accountability for Reasonableness framework is the bare minimum - and yet, 64% of U.S. hospitals still operate in the dark ages. This isn’t ethics, it’s triage theater. We’ve institutionalized moral cowardice under the guise of ‘resource allocation.’ The real scandal? The people who make these decisions are rarely held accountable - and the patients who die from them are erased from the narrative. You don’t get to call yourself a healer if your protocol is a PowerPoint slide buried in a server farm no one reads.
And don’t get me started on the ‘instrumental value’ criterion. Are we really prioritizing nurses over grandmas because they’re ‘useful’? That’s not utilitarianism - that’s fascism with a stethoscope. The ASO guidelines are better, but still flawed. They ignore social determinants. They don’t ask why the patient is even in this situation. Was the drug ever affordable? Was the supply chain ever ethical? Or did we just outsource manufacturing to a factory in Gujarat with a 30% defect rate and call it ‘global efficiency’?
The Mayo Clinic study? Groundbreaking. But only because it proves what we already knew: trauma isn’t a side effect of medicine - it’s the business model. When clinicians are drowning in guilt, the system isn’t broken. It’s working exactly as designed. To produce suffering. To normalize injustice. To make us all complicit in silence.
And let’s not pretend AI will fix this. An algorithm can’t feel the weight of a mother’s cry when her child doesn’t get the drug. It can’t smell the antiseptic in a rural clinic where the IV bag is empty and the nearest pharmacy is 90 miles away. AI doesn’t care about zip codes. But we should. We have to.
This isn’t about rationing. It’s about who we’ve decided is disposable. And if you think this only happens in the U.S., you haven’t been paying attention to India, Nigeria, or rural Ireland. The machine is global. The silence? That’s universal.
So we're supposed to trust a committee of bureaucrats to decide who lives? That's worse than one doctor deciding alone. At least one doctor knows the patient. Committees just read flowcharts while someone dies in the next room.
I’m a nurse in rural Ohio and this hits home. We had a cisplatin shortage last fall. We gave the last vial to a 72-year-old because his daughter cried in the hallway. No committee. No form. Just us, a clipboard, and a prayer. I didn’t know if it was right. But I knew it was human. Maybe the system needs rules - but not at the cost of compassion.
What about the manufacturers? Who’s holding them accountable? Why are there only 3 major players? Why is the FDA letting this happen? Where’s the oversight? Why aren’t we building domestic production? Why aren’t we suing these companies for price-fixing? Why is this even a conversation? This isn’t a shortage - it’s a crime.
Empirical analysis of the Minnesota tiered protocol indicates a statistically significant reduction in inter-hospital variability (p < 0.01). However, the absence of longitudinal data on long-term patient outcomes limits generalizability. Further, the operationalization of 'curative intent' remains semantically ambiguous across oncology sub-specialties.
AI predicting shortages? LOL. The same AI that told you the pandemic was over in 2020? 😂 The real plan? Let the rich buy drugs on the black market and let the rest of us die quietly. They already do this with insulin. Why would this be different?
They want us to trust committees? Nah. We got real Americans out here making real decisions. You think some Ivy League ethicist knows better than a dad who’s been sitting in a hospital for three weeks? No. This is why we lost the country. Too many smart people, not enough tough people.
It is imperative that institutional protocols be standardized, rigorously documented, and subjected to external audit. Failure to do so constitutes a breach of the fiduciary duty owed to patients.
The ethical architecture underpinning contemporary rationing frameworks remains fundamentally incongruent with the Kantian imperative of human dignity. The instrumentalization of life expectancy as a metric is not merely utilitarian - it is ontologically degrading.
India has been dealing with this for decades. We ration because we have to. But we don’t pretend it’s fair. We just do it with prayer, grit, and a lot of chai. No committees. No AI. Just people trying to survive.
You’re all missing the point. The real issue is that we still treat healthcare like a privilege. In Sweden, they just order more. Why can’t we? Because we’re obsessed with profits over people. This isn’t a shortage - it’s a choice.