As of January 2026, more than 287 drugs are still in short supply across the U.S., with nearly half of them being life-saving medications like insulin, chemotherapy agents, and antibiotics. Hospitals are rationing doses. Pharmacies are telling patients to wait weeks. And doctors are forced to use less effective alternatives-sometimes with dangerous results. This isn’t a temporary glitch. It’s a system failure. And Congress is finally trying to fix it.
The Two Bills Trying to Stop the Crisis
Two bills introduced in the 119th Congress are the most direct attempts to tackle this problem. The first is the Drug Shortage Prevention Act of 2025 (S.2665). Introduced by Senator Amy Klobuchar in August 2025, it would require drug manufacturers to notify the FDA the moment they see a spike in demand for critical medicines. Right now, companies aren’t legally required to say anything until it’s too late-often after supplies have already run out. This bill wants to change that by forcing early warnings, giving regulators time to step in, find alternate suppliers, or adjust distribution. The second bill, Health Care Provider Shortage Minimization Act of 2025 (H.R.1160), takes a different angle. It doesn’t focus on pills or injections. It focuses on people. The U.S. is facing a looming collapse in frontline healthcare workers. Over 122 million Americans live in areas where there aren’t enough primary care doctors, nurses, or dentists. The American Association of Medical Colleges predicts a shortage of 124,000 physicians by 2034. H.R.1160 is meant to address that, but here’s the problem: no one knows exactly how. The bill’s full text hasn’t been made public. There are no details on funding, no list of programs it would support, no mention of loan forgiveness, residency expansion, or telehealth incentives. It’s a placeholder with a powerful name-and that’s not enough.Why These Bills Are Stuck
The biggest reason these bills aren’t moving? The longest government shutdown in U.S. history. It started on October 1, 2025, and as of January 2026, it’s still going. Over 800,000 federal workers are furloughed-including the FDA staff who track drug shortages, the HRSA employees who map provider gaps, and the budget analysts who would normally review bills like S.2665 and H.R.1160. The FDA’s Drug Shortage Portal, the main tool hospitals use to check what’s running low, has been down for weeks. Updates aren’t being posted. Alerts aren’t being sent. So even if manufacturers start reporting demand increases under S.2665, there’s no one left to receive the messages. Meanwhile, Congress is busy with other fights. In November 2025, House Republicans pushed to reverse a rule that lets senators sue over phone records. A proposed continuing resolution to keep the government open through January 30, 2026, made no mention of drug shortages or healthcare staffing. No funding. No policy changes. Just a stopgap with no solutions.What’s Really Causing the Shortages?
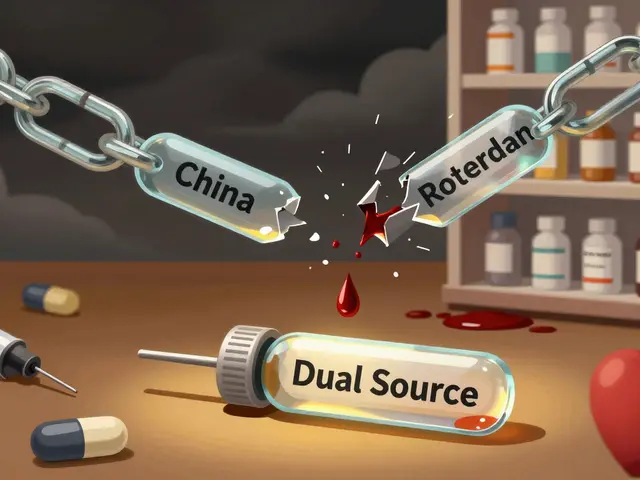
The problem isn’t just bad timing or political gridlock. It’s structural. The Association for Accessible Medicines found that 63% of drug shortages come from manufacturing delays-often because a single factory in India or China makes most of a generic drug, and when that plant shuts down for inspection or supply issues, the whole country feels it. The FDA has limited power to force diversification. Companies don’t see profit in building backup capacity for low-margin generics. And then there’s the workforce side. Medical schools aren’t graduating enough doctors fast enough. Rural clinics can’t compete with urban hospitals on salary. Nurses are quitting after years of burnout. The American Hospital Association reported in October 2025 that 98% of hospitals faced at least one critical drug shortage in the third quarter alone. And 87% of physicians say those shortages directly hurt patient care. Yet only 12% even knew H.R.1160 existed.
The Cost of Doing Nothing
If nothing changes, the damage will keep piling up. The Congressional Budget Office estimates that implementing S.2665 would cost about $45 million a year-just to staff the FDA’s shortage monitoring team. That’s less than 0.003% of the $1.74 trillion federal deficit from 2024-2025. But in a shutdown environment where lawmakers are cutting $1.1 billion from public media and $7.9 billion from foreign aid, even small investments seem impossible. The economic toll is worse. The CBO estimates the shutdown alone is costing the economy $1.5 billion a day. Add to that the hidden costs of delayed surgeries, ER visits for preventable complications, and patients skipping treatments because their meds aren’t available. Those costs don’t show up in budget reports-but they show up in hospital bills, lost wages, and premature deaths.What Could Actually Work?
S.2665 has potential-if it’s done right. But right now, it’s vague. What counts as a “critical drug”? Who pays for the reporting system? What happens if a company lies or delays? Without penalties, this becomes another paperwork requirement with no teeth. Experts say the bill needs three things: clear definitions, mandatory reporting timelines, and fines for noncompliance. H.R.1160 needs more than a name. It needs a plan. The U.S. has successfully reduced provider shortages before-through loan forgiveness for doctors who work in rural areas, expanding nurse practitioner scope of practice, and funding residency slots in underserved regions. If H.R.1160 included even one of those ideas, it would be a real step forward. As it stands, it’s a slogan without a strategy.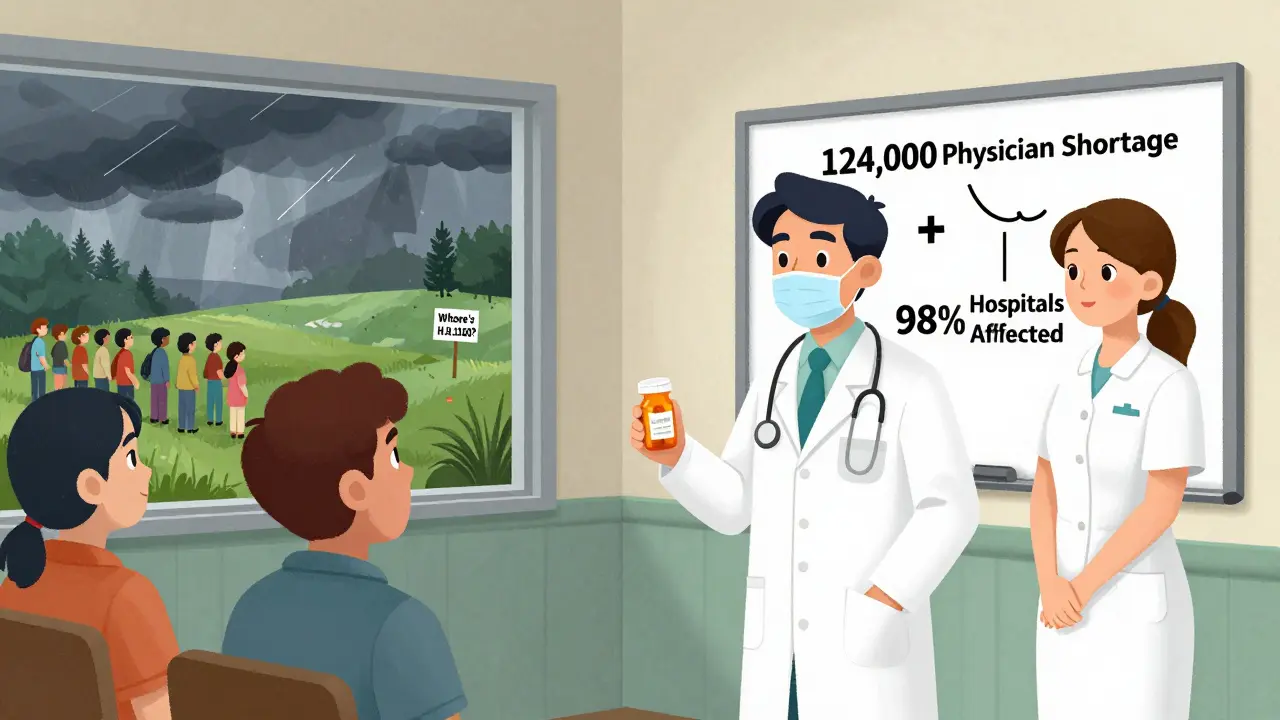
What Patients and Providers Can Do Now
Waiting for Congress isn’t an option. Here’s what you can do:- If you rely on a medication that’s been in short supply, talk to your pharmacist about alternatives. Many generics have interchangeable versions.
- Join patient advocacy groups like the American Society of Health-System Pharmacists or the National Patient Advocate Foundation. They’re tracking shortages and pushing for change.
- Call your representatives. Ask them: “What are you doing about S.2665 and H.R.1160?” If they don’t know, they’re not paying attention.
- Report shortages directly to the FDA’s Drug Shortage Portal-even if it’s slow. Your report might be one of the few still being collected.
There’s no magic fix. But if Congress does nothing, the shortages will keep getting worse. And next time, it won’t just be insulin or antibiotics. It could be the drug that saves your child, your parent, or you.
What is the Drug Shortage Prevention Act of 2025?
The Drug Shortage Prevention Act of 2025 (S.2665) is a Senate bill that would require pharmaceutical manufacturers to notify the FDA when they see a sudden increase in demand for critical drugs. The goal is to give regulators time to respond before supplies run out. It’s designed to fix the current system where companies don’t have to report shortages until after they’ve already happened.
Why hasn’t H.R.1160 been made public?
As of January 2026, the full text of H.R.1160 has not been released to the public. Congressional records only list the bill’s title and number. Without the full text, it’s impossible to know what solutions it proposes, how it would be funded, or whether it includes real strategies to recruit or retain healthcare workers. This lack of transparency has drawn criticism from policy experts and healthcare groups.
How many drugs are currently in short supply?
As of September 30, 2025, the FDA listed 287 drugs in short supply, with 47% classified as “critical”-meaning they treat life-threatening conditions like cancer, heart failure, or severe infections. These numbers haven’t improved since then, and the ongoing government shutdown has made tracking even harder.
Is the government shutdown blocking drug shortage efforts?
Yes. The shutdown, which began in October 2025, has furloughed nearly all FDA staff responsible for monitoring drug supplies. The agency’s Drug Shortage Portal is no longer being updated. Without these workers, even well-written bills like S.2665 can’t be implemented. Legislative progress has stalled across the board.
What can I do if my medication is unavailable?
First, contact your pharmacist-they may know of an alternative brand or generic version. If not, ask your doctor to file a request with the FDA for emergency importation of the drug from another country. You can also report the shortage directly to the FDA’s Drug Shortage Portal. And don’t stop taking your medication without medical advice-some substitutions can be dangerous.



Comments
It's wild how we keep treating this like a glitch instead of a systemic collapse. I've seen nurses scramble for insulin alternatives while parents cry in ER waiting rooms. This isn't political theater-it’s people dying because we chose to look away.
The real tragedy isn't the bills failing-it's that we've normalized this level of neglect. We accept rationing like it's inevitable, not criminal. What does it say about us when the most basic survival meds become lottery tickets?
Let me tell you something they don't want you to know. The FDA shutdown? That's just the tip. Big Pharma owns half the Congress. The real reason S.2665 won't pass is because it'd force them to disclose their global manufacturing chokepoints. They'd rather let kids die than lose a quarter in profit. Watch the FDA portal come back online the moment a candidate mentions Medicare for All.
Okay, real talk: if you’re reading this and you’re not screaming at your rep, you’re part of the problem. I called mine three times last week. Got voicemail each time. So I showed up at their district office with a stack of patient stories. They finally answered. You think it’s hopeless? Try showing up. Try being loud. Try being annoying. We’ve got nothing left to lose.
Also-pharmacists are heroes. If your med’s out, ask them about compounding or foreign equivalents. I got my chemo drug from Canada last month. Legal? Barely. Necessary? Absolutely.
And yes, H.R.1160 is a joke. But we can still push for loan forgiveness for rural nurses. We can still demand more residency slots. We can still vote for anyone who says ‘healthcare is a right’ and actually means it.
Stop waiting for Congress to save us. We’ve got to save each other.
From India, I’ve seen how cheap generics are made. Factories cut corners. FDA inspections? They pay off local officials. This isn’t just an American problem-it’s a global supply chain nightmare. If the U.S. wants real change, it needs to pressure India and China to enforce quality standards, not just ask their own companies to report.
I work in a rural clinic. We’ve been rationing antibiotics since November. Parents drive two hours just to get a script filled. No one’s talking about how this hits the elderly and disabled the hardest. We need action, not just bills with pretty names. And we need it before someone dies because we were too busy arguing about procedure.
It is imperative to underscore the gravity of the situation at hand. The legislative inertia exhibited by the 119th Congress is not merely unfortunate-it is an abdication of the state’s fundamental duty to protect the welfare of its citizenry. The absence of transparency regarding H.R.1160 constitutes a breach of democratic accountability. Furthermore, the systemic underfunding of the FDA is a structural failure that demands immediate remediation through bipartisan fiscal prioritization.
Let’s be precise: S.2665 is a regulatory Band-Aid. Without mandatory reporting timelines, penalties for noncompliance, and a clear definition of 'critical drug,' it’s just another compliance checkbox. And H.R.1160? Zero deliverables. Zero funding. Zero teeth. Meanwhile, the CBO estimates the shutdown costs $1.5B/day. That’s more than the entire federal budget for public health infrastructure. We’re spending billions to keep the lights on while letting the patients die in the dark.
OMG I CRIED reading this. My mom had to switch chemo drugs last month and she got sepsis from the substitute. I’ve been calling senators for months. No one answers. I even emailed the FDA-got an auto-reply saying their portal is down. I’m done waiting. I’m starting a GoFundMe to fly my mom to Canada for her meds. This isn’t just broken-it’s evil.
Here’s what actually works: loan forgiveness for doctors who work in rural areas. We’ve done it before. We’ve got the model. We just need the will. And if you think this is about politics, you’re wrong. It’s about people. My cousin’s kid needed antibiotics. Couldn’t get them. Ended up in ICU for three weeks. That’s not a statistic. That’s my family. We can fix this. But we have to choose to.
Insulin shortages? My brother’s been paying $1200 a month out of pocket since last year. The system isn’t broken-it was designed this way. Profit over people. Always. And now Congress wants to slap a sticker on it and call it a bill? Nah. We need to burn it down and start over. No more compromises. No more waiting. No more silence.
So we’ve got two bills. One’s got a plan but no staff to enforce it. The other’s got a name but no content. And the people who could fix it? They’re on unpaid leave. Meanwhile, the rest of us are just… waiting. Like it’s a Netflix drop. 'Coming soon: a functioning healthcare system.' Yeah right. I’ll believe it when I see it.