When you're producing medical devices, pharmaceuticals, or even high-precision components, your equipment isn't just a tool-it's a measurement system. If your scale reads 10.1 grams when it should read 10.0, that tiny error can mean a batch of pills is underdosed. Or worse, unsafe. That's why calibration and validation aren't optional checklists. They're the backbone of quality control in manufacturing.
What Calibration Actually Means (And Why It's Not Just a Label)
Calibration isn't about sticking a sticker on a device saying "Passed." It's about proving, with data, that your instrument gives accurate readings compared to a known standard. The International Organization for Standardization (ISO) defines it clearly: calibration links your device's readings to a chain of references that ultimately trace back to the International System of Units (SI)-like the kilogram or the meter. This chain must be documented, with each step showing measurement uncertainty.
ISO 13485:2016, the gold standard for medical device manufacturers, says equipment must be calibrated at "specified intervals or prior to use." That means you can't just wait until something breaks. You need a schedule based on risk. A micrometer used to measure heart valve components? Calibrate every three months. A basic thermometer in a warehouse storing packaging materials? Maybe once a year.
And here’s the catch: the calibration standard itself must be traceable. If you're using a weight to calibrate a scale, that weight must have been calibrated by a lab that's traceable to NIST (in the U.S.) or BIPM (in Europe). No traceability? Your entire measurement chain is built on sand. The FDA has issued warning letters over this exact issue-37.2% of them, according to GageList's 2023 analysis.
Validation: Proving Your Equipment Does What It's Supposed to Do
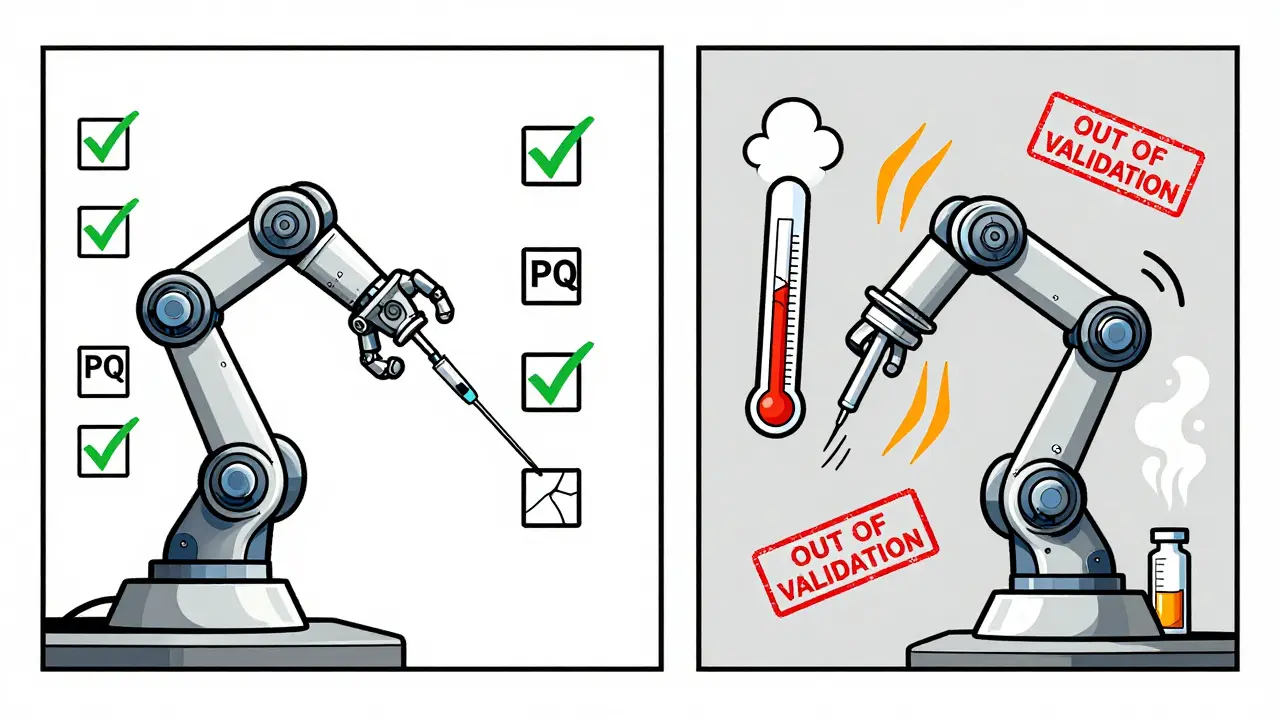
Calibration tells you your instrument reads correctly. Validation tells you it works correctly in your process.
Think of it this way: a thermometer might be perfectly calibrated to read 37°C when placed in a water bath. But if you're using it to monitor a sterilization chamber, you need to know if it can handle the heat, steam, and pressure without drifting. That's validation.
Validation follows three steps: Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ). IQ confirms the equipment was installed right-correct power, connections, environment. OQ tests it under normal operating conditions-does it heat to 121°C and hold it for 30 minutes? PQ proves it consistently produces the right outcome in real production-does every batch meet sterility specs?
For a simple conveyor belt, validation might take a week. For a robotic arm that fills syringes with biologic drugs? It can take 18 to 24 months and cost between $25,000 and $500,000. That’s not an expense-it’s insurance against product recalls and regulatory shutdowns.
How Different Standards Compare (And Where They Clash)
Not all regulations are created equal. ISO 13485:2016 demands 100% traceability to SI units with no exceptions. CLIA, which governs clinical labs, allows some devices-like point-of-care glucose meters-to skip full calibration if they follow manufacturer verification protocols. That’s a 23.5% reduction in workload for waived tests, according to CMS 2023 data.
ISO 9001:2015 lets you extend calibration intervals if you prove your equipment is stable. You might collect data for 18 months and show your pressure gauge never drifts beyond tolerance. ISO 13485 doesn’t let you do that unless you formally validate the extended interval. That’s a major difference.
And then there’s the EU MDR 2017/745. It requires traceability to BIPM standards. The FDA accepts NIST. If you sell globally, you need two calibration records for the same device. That adds 18.7% to compliance costs, according to a McKinsey study of 45 medical device firms.
Why Calibration Fails (And How to Stop It)
Most failures don’t happen because someone forgot to calibrate. They happen because the environment changed.
NIST Technical Note 1900 (2022) found 57.8% of out-of-tolerance incidents occurred when temperature swung more than ±5°C from calibration conditions. A lab calibrated at 20°C, but the production floor hit 28°C. Suddenly, your laser measuring system is off by 0.5%. You don’t know. Your product is out of spec. And you didn’t catch it.
Humidity is another silent killer. In semiconductor manufacturing, 41.3% of calibration failures come from uncontrolled humidity, per SEMI E177-0323. That’s why some shops spend $85,000-$120,000 on ISO Class 5 environmental chambers.
And don’t forget the human factor. A 2024 FDA Small Business Survey found small manufacturers spend 15.2 hours a week just managing calibration paperwork. That’s not time spent improving quality-it’s time spent chasing stamps.
How to Get It Right: A Practical Roadmap
Building a compliant calibration program takes time, but it doesn’t have to be chaotic. Here’s how top manufacturers do it:
- Inventory everything. List every measuring device, from a simple ruler to a CNC machine with embedded sensors. Assign a unique ID to each one.
- Classify by risk. High-risk devices (those affecting product safety) get quarterly checks. Low-risk ones? Annual.
- Use the Method 5 approach. Combine manufacturer recommendations, historical data, and risk assessment. Don’t just go by the manual. If your scale has been stable for 18 months, prove it-and extend the interval.
- Control the environment. Monitor temperature and humidity in real time. If it drifts, flag the last calibration as potentially invalid.
- Go digital. Calibration management software like GageList or Trescal automates scheduling, sends reminders, stores certificates, and generates audit reports. Companies using these tools cut audit prep time by 63.2%.
One biomedical engineer on Reddit extended her lab’s electronic scale calibration from quarterly to biannually after 18 months of stability data. Saved $18,500 a year. No FDA issues. That’s smart risk management.

The Future Is Continuous, Not Periodic
The old model-calibrate once a year, then forget-is dying. The future is continuous verification.
ISO published Amendment 1 to ISO 13485:2016 on March 15, 2024, requiring calibration of AI/ML-based systems through "continuous validation protocols." That means algorithms that predict defects or adjust machine settings must be monitored for drift, not just checked once a year.
The FDA’s 2024 Calibration Modernization Initiative mandates all Class II/III device manufacturers switch to electronic records by December 31, 2026. That’s over 14 million paper records eliminated.
And NIST’s roadmap for quantum-based calibration? It promises 100x more accurate electrical measurements by 2030. That could mean calibrating critical medical sensors every five years instead of every six months.
But here’s the catch: 83.6% of calibration labs report technician shortages. And 47 accredited labs closed in 2023 because they couldn’t hire qualified people. If you’re relying on outside labs, you’re at risk.
The smart move? Build internal capability. Train one person in metrology fundamentals. Get them certified as a Certified Calibration Technician (CCT) through ASQ. That credential is held by over 14,000 professionals globally-and those people earn 22.5% more than non-certified peers.
What Happens If You Ignore This?
You don’t get fined for forgetting to calibrate. You get shut down.
FDA 483 observations, warning letters, consent decrees, recalls-they all start with a measurement error that no one caught. A single faulty sensor can lead to a product recall costing millions. Or worse, harm a patient.
Companies that treat calibration as a cost center lose. Companies that treat it as a risk control system win. They avoid audits. They keep production running. They build trust.
It’s not about doing more paperwork. It’s about knowing your numbers are right-every single time.
How often should equipment be calibrated?
There’s no universal answer. Calibration frequency depends on the equipment, its use, and risk. ISO 13485:2016 requires calibration at "specified intervals or prior to use." High-precision tools in medical device manufacturing are often calibrated every 3-6 months. Basic tools like thermometers in low-risk areas may be calibrated annually. The key is using historical data and risk assessment to justify your intervals-not just following the manufacturer’s default recommendation.
What’s the difference between calibration and validation?
Calibration confirms your instrument reads accurately against a known standard. Validation proves your equipment performs correctly in your specific process. For example, a scale might be calibrated to read 10.00 g accurately. Validation tests whether it consistently dispenses the right dose into a vial under real production conditions, including vibration, temperature, and operator handling.
Do I need to calibrate every piece of equipment?
No. Only equipment that affects product quality, safety, or regulatory compliance needs calibration. A stapler? Probably not. A torque wrench that tightens a critical screw on a pacemaker? Absolutely. Start by mapping your processes and identifying which measurements directly impact your output. That’s your calibration scope.
Can I extend calibration intervals if my equipment is stable?
Yes, but only if you have data to prove it. ISO 9001:2015 allows this. ISO 13485:2016 requires formal validation of the extended interval. Collect at least 12-18 months of calibration records showing the device stayed within tolerance. Document your risk assessment. Then, get approval from your quality team. Many labs have saved thousands by doing this-without sacrificing safety.
What happens if I skip calibration?
You risk product non-conformance, regulatory action, or worse-patient harm. The FDA cited inadequate calibration in 37.2% of warning letters in 2023. A single out-of-tolerance measurement can lead to a recall, production halt, or even a consent decree. The cost of fixing it later is always higher than the cost of maintaining a program.
Is calibration software worth the investment?
For any manufacturer with more than 20 measuring devices, yes. Software like GageList or Trescal automates scheduling, tracks certificates, sends reminders, and generates audit-ready reports. Companies using these tools reduce audit prep time by over 60%. For small manufacturers, it cuts administrative burden from 15+ hours per week to under 5. The ROI is clear: less stress, fewer errors, faster audits.
Calibration and validation aren’t about checking boxes. They’re about confidence. Confidence that your product works. Confidence that your customers are safe. Confidence that your facility passes inspection. Start with your most critical equipment. Build your process. Let data guide you. And don’t wait for the FDA to remind you why it matters.


