When you pick up a prescription, the bottle might say omeprazole - but you’ve heard it called Prilosec. Or maybe it says atorvastatin, but your doctor called it Lipitor. It’s confusing. And if you’ve ever stared at a pill and thought, Is this really the same thing? - you’re not alone.
Why Two Names? The Basics
Every prescription drug has two names: a generic name and a brand name. The generic name is the active ingredient - the chemical that actually does the work in your body. The brand name is the trademark the company made up to sell it. Think of it like soda: carbonated water, high fructose corn syrup, caramel color, phosphoric acid is the generic list of ingredients. Coca-Cola is the brand. The FDA requires that generic drugs contain the exact same active ingredient, in the same strength, and in the same form (tablet, capsule, liquid) as the brand-name version. That means if your brand-name drug has 20mg of omeprazole, the generic has 20mg of omeprazole. No more, no less.Are Generics Really the Same?
Yes. But not exactly. The FDA doesn’t just say generics are equal - they prove it. Before a generic drug can be sold, the manufacturer must show it’s bioequivalent to the brand-name drug. That means the amount of medicine your body absorbs, and how fast it gets there, must fall within a tight range: 80% to 125% of the brand-name version. This isn’t a guess. It’s tested in real people using blood samples over time. A 2022 analysis by University Hospitals found that 90% of all prescriptions filled in the U.S. are for generic drugs. That’s not because pharmacies are pushing them - it’s because patients and insurers choose them. And for good reason: generics cost 80% to 85% less. Lipitor (brand) used to run $300 a month. Atorvastatin (generic)? Around $4. Even the FDA says it: “Generic drugs are safe, effective, and of high quality - all at substantial savings.”What’s Different? (And Why It Matters)
The active ingredient? Identical. The rest? Not always. Generic pills can look different. They might be a different color, shape, or size. That’s not a mistake - it’s the law. Trademark rules stop generic makers from copying the exact appearance of brand-name pills. So if you’ve always taken a blue oval pill and now get a white round one, it’s still the same medicine. Just packaged differently. The inactive ingredients - things like dyes, fillers, and coatings - can vary. For most people, this doesn’t matter. But for some, it can cause minor reactions. A person with a corn allergy might react to a filler made from corn starch. Someone with sensitive stomachs might notice a different coating changes how fast the pill dissolves. This is why some patients report feeling “different” after switching. It’s rarely the active ingredient. It’s the extras. Talk to your pharmacist if you notice changes in side effects after switching to a generic.Narrow Therapeutic Index Drugs: The Exception
There’s one group of drugs where even tiny differences matter: narrow therapeutic index (NTI) drugs. These are medications where the line between helping you and hurting you is thin. Examples include warfarin (a blood thinner), levothyroxine (for thyroid), and some seizure meds. For these, the FDA still approves generics - but some doctors prefer to stick with the brand name, especially when starting treatment or adjusting doses. Why? Because even a 5% variation in absorption could mean your blood doesn’t clot right, or your thyroid levels go off. It’s rare - less than 1% of all medications fall into this category - but it’s real. If you’re on one of these, ask your doctor: “Is it safe to switch?”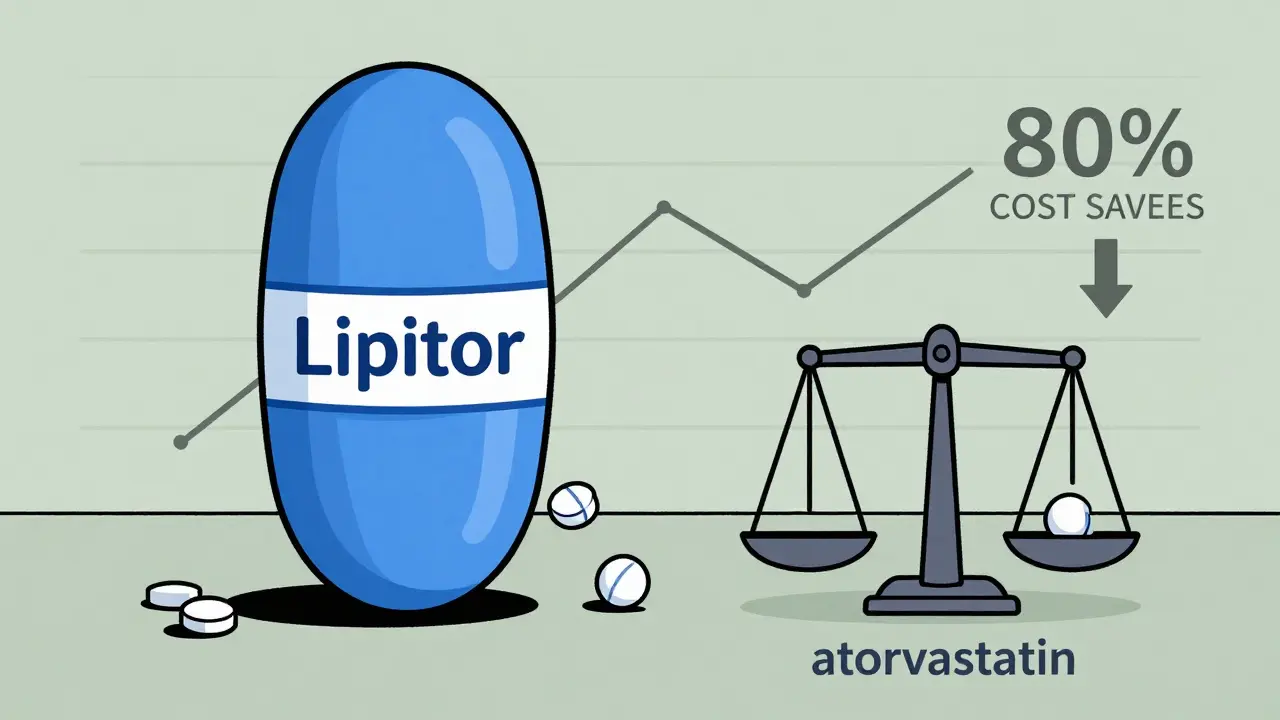
How to Read Your Prescription Label
Your pill bottle should clearly show both names. The brand name is usually bigger, on top. The generic name is smaller, underneath. For example:- Prilosec (brand)
- omeprazole (generic)


Comments
OMG I switched from Prilosec to omeprazole and thought I was dying-my stomach was doing backflips for three days. Turns out? The coating on the generic was made with corn starch and I’m allergic. My pharmacist was like, ‘Sweetie, you need the one with the rice filler.’ Now I’m on a $3 version that doesn’t make me feel like I swallowed a cactus. Also, why does Big Pharma make us feel guilty for saving money? 🤡
It’s not just about the active ingredient-it’s about integrity. If you’re taking a generic, you’re gambling with your health. The FDA’s ‘bioequivalence’ range of 80%-125% is a joke. That’s a 45% swing! Would you let a pilot fly if their altitude could be off by 45%? No. So why are you swallowing pills that could be half as strong-or worse? You’re not saving money. You’re risking your life.
It is imperative to recognize, from a pharmacoeconomic and regulatory standpoint, that the FDA’s ANDA (Abbreviated New Drug Application) pathway is not a lesser standard-it is a scientifically rigorous, statistically validated mechanism for ensuring therapeutic equivalence. The bioequivalence parameters (Cmax, AUC) are not arbitrary thresholds; they are anchored in population pharmacokinetic modeling and validated through crossover trials with a power of ≥80%. To conflate appearance with efficacy is a profound misunderstanding of pharmaceutical science.
Who cares what the pill looks like? If you’re still paying $300 for Lipitor when you can get atorvastatin for $4, you’re either rich or an idiot. I’ve been on generics since 2018. My blood pressure is better. My wallet is happier. And no, I didn’t turn into a zombie. Stop being scared of a white pill because it’s not blue. You’re not special. The medicine works. Move on.
I used to be terrified of generics too-until I started talking to my pharmacist. She showed me the FDA’s database and explained how the inactive ingredients are listed. I had no idea some fillers could cause reactions. Now I always ask for the ‘corn-free’ version of my thyroid med. It’s not about distrust-it’s about knowing your body. And honestly? The people who say generics don’t work? They never asked their pharmacist a single question.
generic = same medicine, cheaper. brand = same medicine, plus fancy packaging and ads. i switched to generic sertraline and still feel like me, just with more cash in my pocket. no drama. no magic. just science. also, my pill is now green. weird, but fine.
Why do we even let foreign companies make our meds? Like, I get the cost thing, but what if the generic is made in a factory with no oversight? I don’t trust Chinese or Indian labs. I’d rather pay $100 for Lipitor than risk my life because someone cut corners overseas. America first, even in pills.
my aunt was scared to switch to generic levothyroxine too. we went to the pharmacy together and she asked the pharmacist to show her the batch number and the testing report. she felt better after knowing the truth. sometimes, just knowing helps more than the pill itself. 🤍
GENERIC = 💰💰💰
BRAND = 😭💸💸
ME AFTER SWITCHING = 😌😌😌
Also, my pill is now a rainbow. I call it my ‘happy pill’ 😊
While I appreciate the data presented, I would respectfully suggest that the emotional response to pill appearance is not trivial. Psychological factors, including placebo and nocebo effects, are clinically significant in chronic medication adherence. The perceived difference may not be pharmacological-but it is real, and should be acknowledged with empathy, not dismissal.
My mom switched to generic warfarin and had a minor bleed. Not because it was weaker-but because the timing of absorption was slightly different. She went back to brand. Not because she’s paranoid. Because she’s 78 and doesn’t want to risk it. We need options, not pressure.
In India, generics are the only option for most people. I’ve seen patients with diabetes, hypertension, epilepsy-living full lives on $1/month meds. The fear of generics is a luxury of wealth. The real question isn’t whether they work-it’s why we make people feel guilty for using them when they’re safe, legal, and life-saving.
bro i took generic adderall once and felt like a ghost. switched back to brand. my brain works better. not saying generics are bad. just saying… some bodies react weird. ask your doc before you gamble.
Wow. A 1200-word essay on how a pill is still a pill. Groundbreaking. I’m sure Big Pharma is weeping into their $300 Lipitor bottles right now. 😭