What Exactly Are Hives?
Hives, or urticaria, are raised, itchy welts that appear suddenly on the skin. They can be as small as a pinhead or as large as a dinner plate. These red or skin-colored bumps often look like nettle stings - which is why they’re sometimes called nettle rash. They come and go, sometimes fading in one spot only to pop up somewhere else. What makes them so frustrating is how unpredictable they are. One day you’re fine, the next you’re covered in angry, burning patches that won’t stop itching.
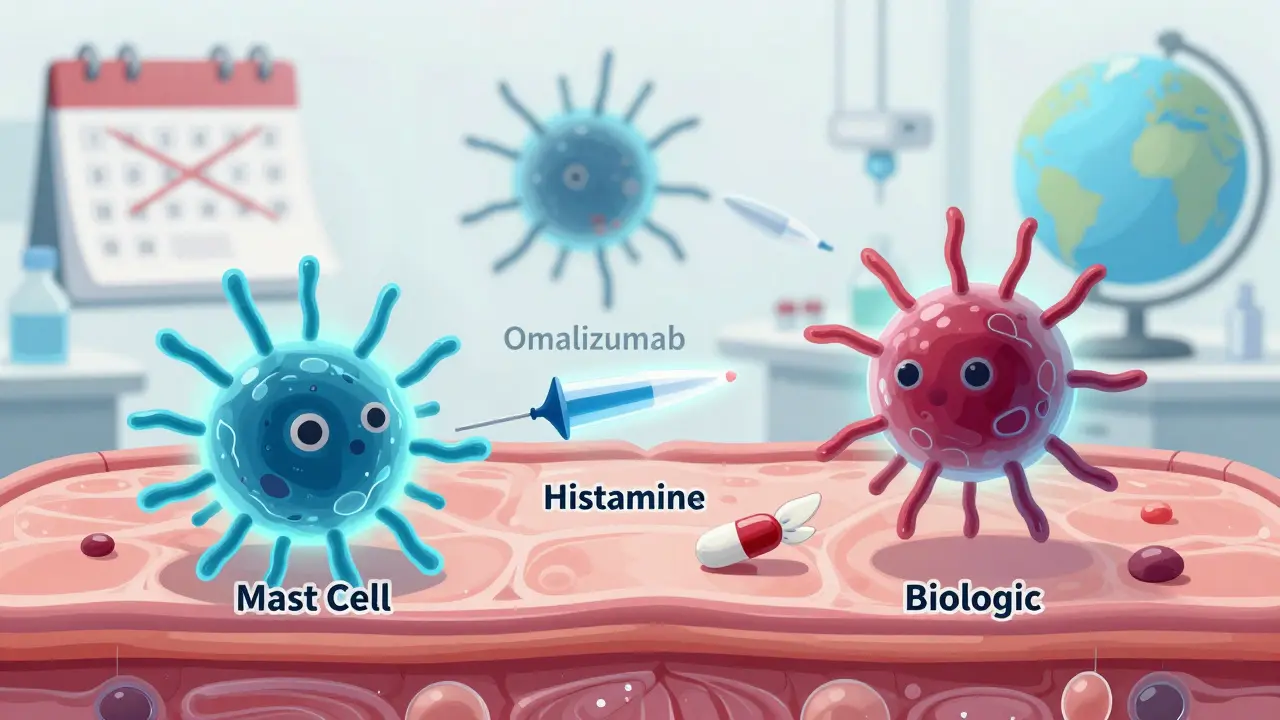
The cause? Your body’s mast cells release histamine, a chemical that makes blood vessels leak fluid into the skin. That fluid creates the swelling and itch. It’s an overreaction - like an alarm going off when there’s no fire. Most cases last less than six weeks (acute urticaria). But if they stick around longer, it’s called chronic spontaneous urticaria (CSU), which affects about 1 in 50 people at some point. Women are more likely to get it than men, and it often starts between ages 20 and 50.
What Triggers Hives?
Not all hives are caused by allergies. In fact, only about 10% of chronic cases have a clear allergic trigger. Common culprits include:
- Food: nuts, shellfish, eggs, dairy, and food additives like sulfites or artificial colors
- Medications: antibiotics like penicillin, NSAIDs like ibuprofen, and even aspirin
- Insect stings or bites
- Physical triggers: pressure, heat, cold, sunlight, or sweat - these are called physical urticarias and make up 20-30% of chronic cases
- Infections: viruses like colds or hepatitis, or even bacterial infections like strep throat
- Stress and hormonal changes
Here’s the catch: in 70-80% of chronic cases, doctors can’t find any trigger at all. That’s called idiopathic urticaria. It doesn’t mean nothing’s causing it - it just means current tests can’t detect it. Autoimmune reactions, where your immune system attacks your own skin cells, are suspected in many of these cases.
Antihistamines: The First Line of Defense
When you get hives, the go-to treatment is almost always an antihistamine. These drugs block histamine from binding to receptors in your skin, which stops the itching, swelling, and redness. There are two main types:
- Second-generation: Cetirizine (Zyrtec), loratadine (Claritin), fexofenadine (Allegra). These don’t make most people sleepy and last 24 hours. Dose: 10mg once daily for adults.
- First-generation: Diphenhydramine (Benadryl), hydroxyzine. These work fast but cause drowsiness in 50-70% of users. They’re better for nighttime use if itching keeps you awake.
Many people think one pill a day is enough. But for chronic hives, that’s often not enough. The 2023 international guidelines say you should increase the dose - up to four times the standard amount - before trying anything else. For example, taking 40mg of cetirizine daily (four 10mg tablets) can help where 10mg failed. About half of people with chronic hives respond to this approach.
Real-world feedback supports this. On WebMD, users report cetirizine gives 8-10 hours of relief. But others say loratadine wears off after 4-6 hours, forcing them to take it twice a day. That’s why some doctors recommend combining a non-drowsy antihistamine during the day with a sedating one at night. Studies show this combo improves control by 30%.

What If Antihistamines Don’t Work?
If you’ve tried high-dose antihistamines for months and still break out daily, it’s time to consider stronger options. The next step is usually a biologic - a targeted drug made from living cells.
Omalizumab (Xolair) has been used since 2014. It’s an injection given every four weeks under the skin. In clinical trials, 65% of patients who didn’t respond to antihistamines saw their hives disappear. Users on PatientsLikeMe report 72% satisfaction. But it’s expensive - around $1,500 per shot - and can cause injection site reactions.
In September 2023, the FDA approved dupilumab (Dupixent) for chronic hives. It’s another injectable, originally for eczema and asthma. In trials, 55% of users had complete symptom control versus 15% on placebo.
Then came remibrutinib, approved in January 2024. This is the first oral drug in its class - a tyrosine kinase inhibitor. It’s taken as a pill twice a day. In trials, 45% of users had complete symptom control. The big advantage? No needles. Patient adherence is 85% with pills versus 70% with injections.
Other options like cyclosporine or short-term steroids (prednisone) are still used, but with caution. Steroids can clear hives fast, but after just three days, 35% of users develop high blood sugar, 25% get insomnia, and 20% feel moody or anxious. Cyclosporine helps 54-73% of tough cases, but it can damage kidneys or raise blood pressure. These are last-resort treatments.
Living With Chronic Hives
Chronic hives don’t just hurt your skin - they wreck your sleep, mood, and daily life. On Reddit’s r/ChronicHives community, 68% of 1,245 members said hives disrupted their sleep, with 42% waking up 2-3 times a night from itching. That kind of exhaustion leads to anxiety and depression. The European Academy of Dermatology found 15-20% of chronic hives patients develop these mental health issues.
Tracking your symptoms helps. Use a simple diary: note what you ate, where you were, how you felt, and when the hives appeared. Apps like Urticaria Tracker (rated 4.3/5 on the App Store) make this easier. Some people find relief by avoiding known triggers - like switching to fragrance-free soaps, wearing loose clothes, or cooling down after exercise.
But if you can’t find a trigger - and most can’t - don’t blame yourself. This isn’t your fault. It’s your immune system misfiring.
What’s Next for Urticaria Treatment?
The field is moving fast. Researchers are testing new oral drugs that target different parts of the immune system. Linzagolix, expected for FDA review in late 2024, showed 52% complete response in early trials. Scientists are also exploring genetic testing to predict which antihistamine will work best for you - before you even take it. The goal? Personalized treatment based on your biology, not trial and error.
Access remains unequal. In wealthy countries, 85% of chronic hives patients can get biologics. In low-income regions, it’s only 30%. Telemedicine is helping bridge the gap - 45% of U.S. allergists now use video visits, making specialist care more accessible to people in rural areas.
When to See a Doctor
Start with an over-the-counter antihistamine if you get hives once or twice. But if they last more than two weeks, or if you’re breaking out daily, see an allergist. Don’t wait. Many people see three or more doctors before getting the right diagnosis. Early intervention prevents unnecessary suffering and opens the door to better treatments sooner.
Also, if you have swelling in your lips, tongue, or throat - or trouble breathing - that’s angioedema. Call 911. It’s not just hives. It can be life-threatening.
Bottom Line
Hives are common, often misunderstood, and rarely dangerous - but they can be debilitating. Antihistamines are your first tool, but they’re not the only one. High doses, combination therapy, and newer biologics can bring real relief. You don’t have to live with daily itching. There are options. The key is persistence, tracking, and finding a doctor who knows the latest guidelines. Chronic hives aren’t curable yet - but they’re manageable. And that’s more than enough to get your life back.


