Every year, millions of people in the U.S. take medications without issue. But for some, a simple pill or injection triggers a reaction that can go from mild to life-threatening in minutes. The problem? Most people don’t know if it’s a side effect-or a true drug allergy. And mislabeling yourself as allergic can cost you more than just a few days of discomfort-it can lead to worse treatments, longer hospital stays, and even avoidable deaths.
What’s the Difference Between a Side Effect and an Allergy?
Not every bad reaction to a drug is an allergy. A side effect, like nausea from antibiotics or drowsiness from painkillers, is a known pharmacological response. It’s predictable, often listed on the label, and doesn’t involve your immune system.
A true drug allergy? That’s your immune system treating the medication like an invader. It kicks off a chain reaction-releasing histamine and other chemicals-that causes symptoms ranging from a itchy rash to shutting down your lungs and blood pressure. According to the National Institutes of Health, allergic reactions are actually uncommon, but mislabeling is everywhere. About 10% of Americans think they’re allergic to penicillin, but over 90% of them can take it safely after proper testing.
Common Signs of a Drug Allergy
The most frequent sign? A rash. But not all rashes are the same. Here’s how to tell what you’re dealing with:
- Hives-raised, red, itchy welts that come and go. They often appear within an hour of taking the drug.
- Itching-without a visible rash. This can be the first warning, especially with drugs like penicillin or sulfa antibiotics.
- Swelling-in your lips, tongue, throat, or around your eyes. This is called angioedema. It doesn’t always come with hives, but when it does, it’s a red flag.
- Difficulty breathing-wheezing, tightness in the chest, or feeling like you can’t get air in. This isn’t just a cold. It’s your airways reacting.
- Flu-like symptoms-fever, swollen lymph nodes, joint pain. These show up days or weeks later and can point to something like DRESS syndrome or serum sickness.
- Blisters or peeling skin-especially around your mouth, eyes, or genitals. This could be Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN), both medical emergencies.
The Mayo Clinic says serious reactions often start within an hour. But delayed reactions? They can sneak up. A rash from amoxicillin might not show up until day five. That doesn’t make it less dangerous.
When It’s an Emergency: Anaphylaxis
Anaphylaxis isn’t just a bad reaction. It’s a full-body shutdown. The American College of Allergy, Asthma, and Immunology defines it as a reaction that hits two or more body systems at once. Think: hives + vomiting + trouble breathing + dizziness. Or swelling + low blood pressure + chest pain.
If you or someone else has these symptoms after taking a drug:
- Call 911 immediately.
- If you have an epinephrine auto-injector (EpiPen), use it now.
- Don’t wait to see if it gets better. It won’t. Not without treatment.
- Even if you feel better after the shot, you still need to go to the ER. A second wave of symptoms can hit hours later.
Emergency rooms treat anaphylaxis with epinephrine, oxygen, IV fluids, and sometimes steroids. Delayed treatment increases the risk of death. Don’t gamble with it.
Delayed Reactions You Can’t Ignore
Not all drug allergies strike fast. Some take days-or weeks-to show up. These are harder to connect to the medication, but just as dangerous.
- DRESS syndrome (Drug Rash with Eosinophilia and Systemic Symptoms): Starts with a rash, then fever, swollen glands, liver inflammation, and high white blood cell counts. It can damage your organs. If you’ve been on an anticonvulsant, allopurinol, or certain antibiotics and feel sick weeks later, get checked.
- Serum sickness-like reaction: Rash, fever, joint pain, swollen lymph nodes. Usually appears 1-3 weeks after starting the drug. Common with cefaclor or some antivirals.
- Stevens-Johnson Syndrome (SJS) and TEN: These are rare but deadly. Blisters form on your skin and mucous membranes (mouth, eyes, genitals). Skin peels off in sheets. SJS affects less than 10% of your skin; TEN affects more than 30%. Both need ICU care. If you see blisters or peeling skin after a new drug, don’t wait-go to the ER.
What to Do If You Suspect a Drug Allergy
First, stop the drug-unless you’re told otherwise by a doctor. Some meds, like seizure or heart drugs, can’t be stopped suddenly.
Take pictures of any rash, swelling, or blistering. Write down:
- What drug you took
- When you took it
- How long until symptoms started
- What symptoms you had
- How long they lasted
Then, contact your doctor. If it’s not an emergency, they’ll likely refer you to an allergist. Don’t rely on online searches or old stories from friends. This isn’t guesswork-it’s science.
Testing for Drug Allergies: What’s Available
Here’s the hard truth: for most drugs, there’s no blood test or simple lab check. The exception? Penicillin.
For penicillin allergy, allergists use skin testing: a tiny drop of penicillin is placed under your skin. If you’re allergic, a red, itchy bump forms. If that’s negative, they may do an oral challenge-giving you a small, controlled dose of penicillin while watching you closely. It’s safe when done right.
For other drugs, testing is limited. Blood tests can help with DRESS or severe delayed reactions, but they’re not definitive. The best tool? Your detailed history. That’s why documenting your reaction matters so much.
UCLA Health says: if you can’t see your doctor right away, take photos. Those images help specialists make the call.
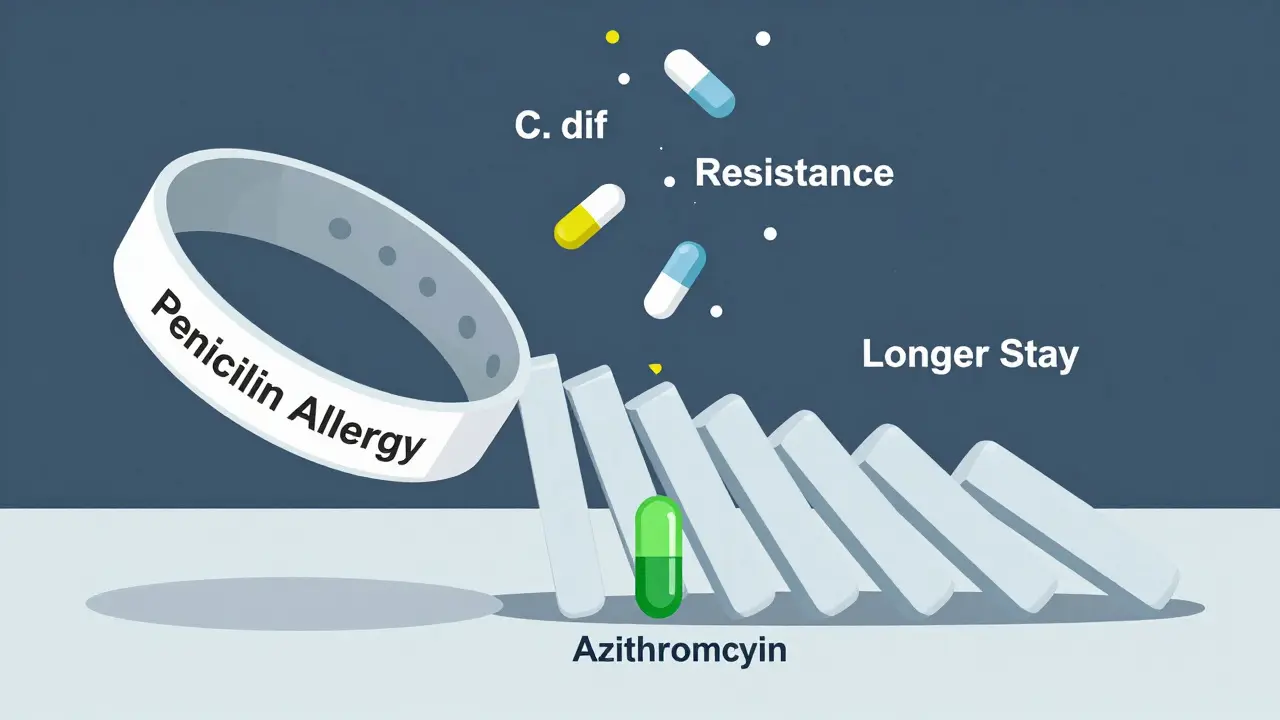
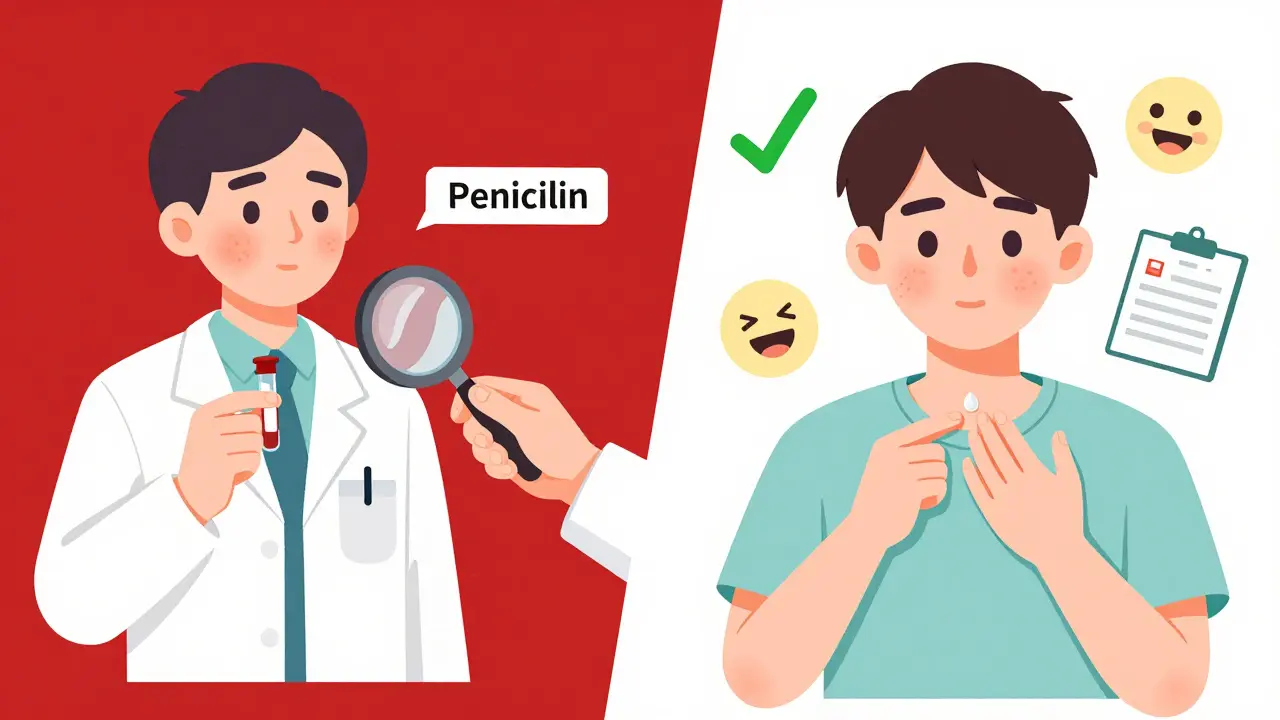
Why Mislabeling Is a Big Problem
If you’re labeled allergic to penicillin-when you’re not-you’re more likely to get stronger, costlier antibiotics. Those drugs increase your risk of deadly infections like C. diff. They’re also harder on your body and more likely to cause resistance.
And it’s not just penicillin. People avoid sulfa drugs, NSAIDs, and even chemotherapy drugs because of old rashes or vague symptoms that weren’t allergies at all. The NIH says mislabeling drives up public health costs and leads to worse outcomes.
Getting tested isn’t just about comfort-it’s about getting the right care when you need it most.
What to Do After Diagnosis
If you’re confirmed allergic to a drug:
- Wear a medical alert bracelet or necklace listing your allergy.
- Keep a written list of drugs you’re allergic to and share it with every doctor, dentist, and pharmacist.
- Ask for alternatives. If you’re allergic to penicillin, ask if azithromycin or cephalexin is safe for you.
- Never assume a new drug is safe just because it’s in the same class. Cross-reactivity happens.
If you’ve had a severe reaction, your allergist may recommend carrying an epinephrine auto-injector-even if you’ve never needed it before. Better safe than sorry.
Final Thought: Trust Your Body, But Verify
Drug allergies are rare. But when they happen, they’re serious. Don’t brush off a rash. Don’t ignore swelling. Don’t assume you’re just "sensitive" to meds.
If something feels wrong after taking a new drug, listen to your body. Document it. Get it checked. And if you’ve been told you’re allergic to penicillin or another common drug-ask if you’ve been tested. You might be able to take it safely. And that could save your life down the road.