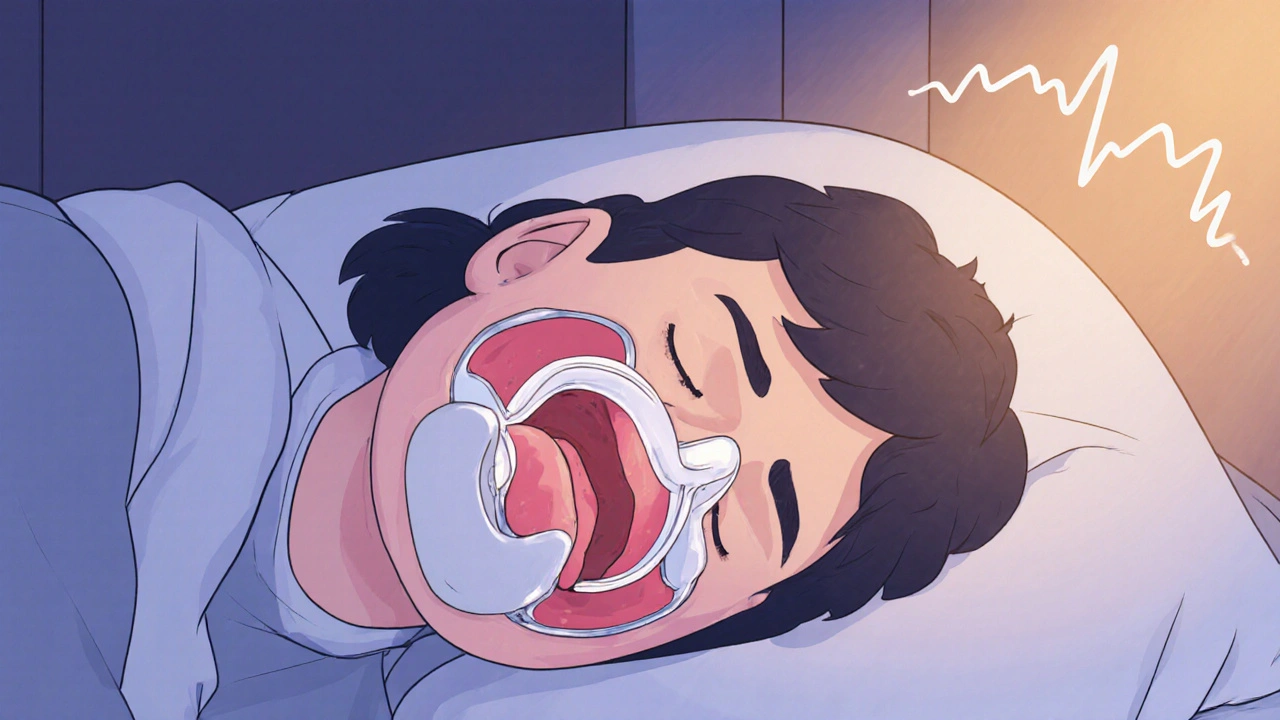
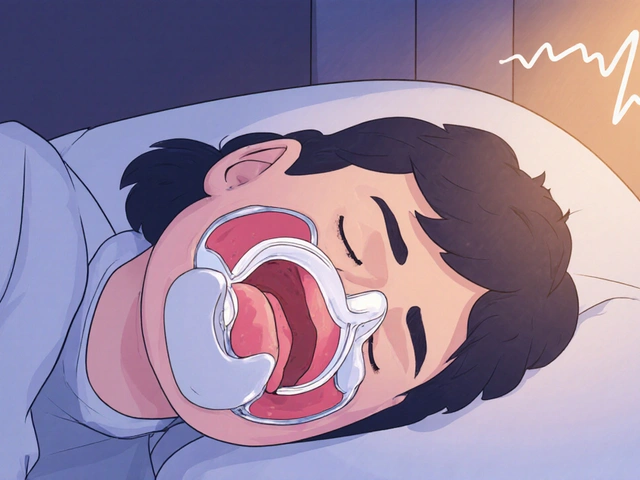
Snoring isn’t just annoying-it can be a sign your airway is collapsing while you sleep. If you’ve tried nasal strips, pillow adjustments, or even sleeping on your side with no real change, you might be wondering: is there something more effective? Mandibular advancement devices (MADs) are one of the most proven, non-invasive solutions for snoring-and they’re growing in popularity fast. Unlike CPAP machines, they don’t require masks, hoses, or air pressure. Instead, they gently move your lower jaw forward to keep your airway open. For many people, this means quieter nights, better sleep, and fewer complaints from their partner.
How Mandibular Advancement Devices Actually Work
Mandibular advancement devices are custom-fitted oral appliances, similar to mouthguards, that hold your lower jaw slightly forward during sleep. This forward position prevents the soft tissues in your throat-like the tongue and uvula-from collapsing backward and vibrating, which is what causes snoring. The science behind it is straightforward: when your jaw moves forward, your airway opens up. Studies show that even a 5-10mm shift can make a big difference.
Most prescription MADs are made from semi-rigid acrylic with titanium connectors, designed to last for years. They’re adjustable, letting your dentist fine-tune the jaw position in small 0.5mm increments. Over-the-counter versions exist too-made from thermoplastic that you boil and bite into-but they’re less precise and often less effective. A 2015 meta-analysis found custom devices reduced snoring by 72.3%, while over-the-counter ones only hit 48.6%.
These devices don’t cure snoring-they manage it. If you stop wearing them, snoring typically returns within two days. But for people who can’t tolerate CPAP, or who have mild-to-moderate sleep apnea, MADs offer a practical, portable alternative. They weigh less than an ounce, fit in a small case, and work anywhere-even on a plane or in a hotel.
Who Benefits Most from Oral Appliance Therapy?
Not everyone who snores is a good candidate. MADs work best for people with:
- Primary snoring (no sleep apnea), or mild-to-moderate obstructive sleep apnea
- At least 6-8 natural teeth in both upper and lower jaws
- Healthy temporomandibular joints (TMJ)-no severe arthritis or joint pain
- No advanced gum disease or loose teeth
Patients with severe anatomical blockages-like those with Mallampati Class IV airways (where the throat is very narrow)-often don’t benefit. In fact, studies show failure rates hit nearly 40% in these cases. That’s why a sleep study (either at home or in a lab) is required before getting a MAD. You need to rule out severe sleep apnea, which might need CPAP or surgery instead.
People who travel often, work irregular hours, or dislike the bulk and noise of CPAP machines tend to do very well with MADs. One Reddit user reported his wife’s snoring dropped from 65dB to 38dB after using a custom device-loud enough to wake her up, but quiet enough to sleep through.
Effectiveness Compared to Other Treatments
How do MADs stack up against other options? Here’s what the data says:
| Treatment | Snoring Reduction | Adherence Rate (12 Months) | Key Limitations |
|---|---|---|---|
| Mandibular Advancement Device (custom) | 65-75% | 76.4% | Requires dental fitting; possible jaw changes over time |
| Mandibular Advancement Device (OTC) | 30-50% | 58.1% | Less precise; higher risk of discomfort |
| CPAP Machine | 85-95% | 45.2% | Mask discomfort, noise, claustrophobia |
| Nasal Dilators | 20-30% | 62.5% | Only helps if nose is the main issue |
| Positional Therapy | 35-45% | 51.3% | Works only if snoring is position-dependent |
CPAP is still the gold standard for stopping snoring completely-but most people can’t stick with it. About half of users quit within a year. MADs, on the other hand, have much higher long-term use rates. That’s why the American Academy of Sleep Medicine recommends them as a first-line treatment for mild-to-moderate sleep apnea and primary snoring.

Side Effects and Long-Term Risks
There’s no such thing as a perfect solution, and MADs come with trade-offs. The most common issues during the first few weeks are:
- Morning jaw pain or soreness (reported by 68% of users)
- Excessive saliva production
- Tooth discomfort or pressure
Most of these fade after 2-4 weeks. Dentists often recommend wearing the device for an hour or two during the day to get used to it before sleeping with it. Warm water soaks can help soften thermoplastic components during adjustments.
The bigger concern is long-term dental changes. About 25% of people who use MADs for five or more years develop permanent shifts in their bite. Some need orthodontic work later. A 2023 study from SUNY warned that these changes can be irreversible. That’s why regular dental check-ups every six months are non-negotiable. Your dentist needs to monitor your teeth, gums, and jaw joint.
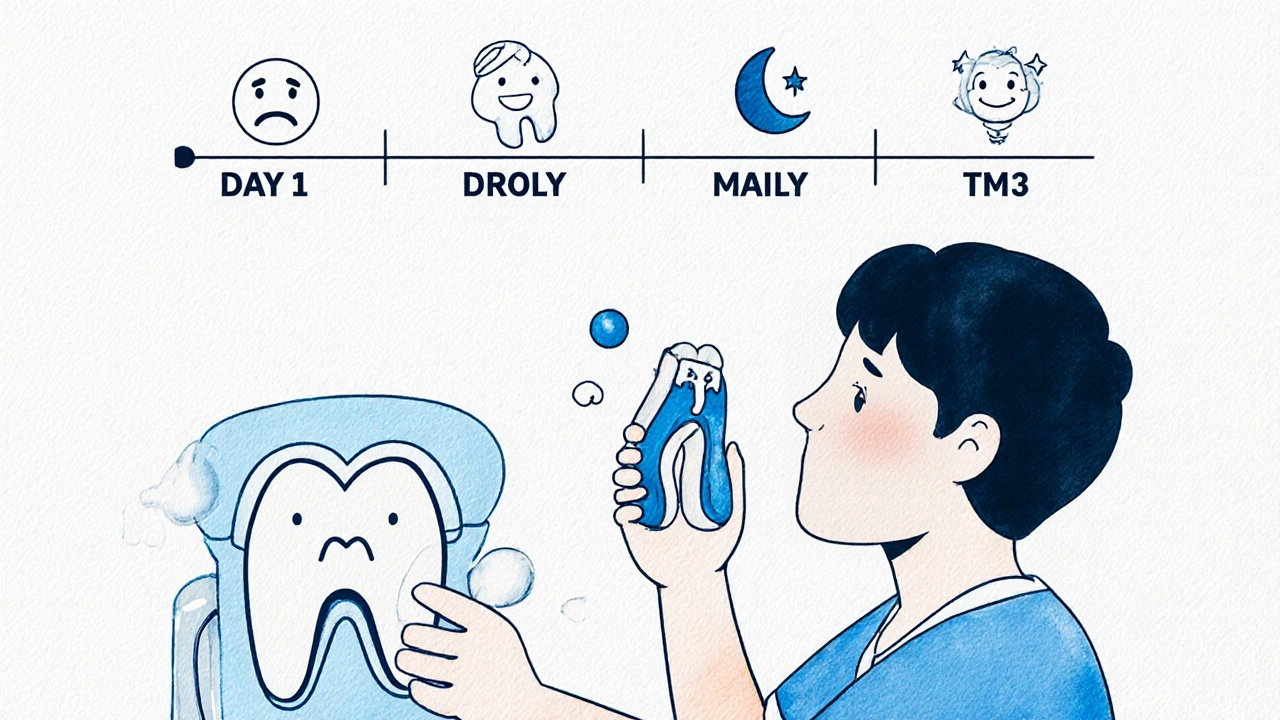
It’s also important to clean the device daily. Left uncleaned, bacteria and plaque can build up, leading to bad breath or even gum infections. Most users rinse theirs with water after each use and soak them weekly in a denture cleaner.
The Process: From Diagnosis to Daily Use
Getting a MAD isn’t as simple as ordering one online. Here’s what the real process looks like:
- Sleep study: Get a home sleep test or in-lab polysomnography to confirm snoring isn’t caused by severe sleep apnea.
- Dental evaluation: Your dentist checks your teeth, gums, jaw joints, and bite. If you have missing teeth or severe periodontal disease, you may not qualify.
- Dental impressions: A custom mold is made-either using traditional putty or digital scanning. Digital scans are 23% more accurate, according to a 2022 study.
- Device fabrication: The appliance is made in a lab and usually ready in 2-3 weeks.
- Titration phase: You start with minimal jaw advancement and increase it by 1mm every 3-5 days over 4-6 weeks until snoring stops or you hit your max comfortable position.
- Follow-ups: You’ll need 2-3 visits over the first few months to adjust fit and check for side effects.
Most people are using the device consistently by day 30. The first week is the hardest-many report feeling like they’re wearing a mouthful of plastic. But after that, it becomes routine.
Cost, Insurance, and Market Trends
Custom MADs cost between $1,800 and $2,500. Over-the-counter versions run $50-$100-but they’re far less effective and often cause more discomfort. Only about 38% of U.S. private insurance plans cover MADs, meaning most people pay out of pocket.
That’s changing. The global market for oral appliances is expected to grow from $1.28 billion in 2022 to $2.41 billion by 2030. More insurers are starting to recognize the long-term savings: people who snore less sleep better, have fewer accidents, and visit doctors less often. Some employers now offer sleep health benefits that include MAD coverage.
Leading brands include SomnoDent MAS, TAP 3, and the newer SomnoDent EVO 3, which has a built-in sensor that connects to an app to track usage and snoring levels. In 2024, a new AI-powered device from Sleep Solutions Inc. will launch, using algorithms to recommend optimal jaw settings based on your breathing patterns.
Is It Worth It?
If you snore loudly, wake up tired, or have a partner who’s had enough-then yes, it’s worth exploring. MADs aren’t magic. They require commitment, dental visits, and ongoing care. But for the right person, they’re life-changing.
Think about it: if you’re paying $2,000 for a device that lets you sleep through the night without waking yourself or your partner, and you use it for five years, that’s less than $400 a year. Compare that to the cost of lost sleep, daytime fatigue, relationship strain, or even the long-term health risks of untreated sleep apnea.
The key is choosing the right path: get evaluated properly, avoid cheap knockoffs, and work with a dentist trained in sleep medicine. Don’t just buy one online and hope for the best. The difference between a custom device and an over-the-counter one isn’t just price-it’s effectiveness, comfort, and safety.
Snoring doesn’t have to be normal. You don’t have to live with it. And you don’t have to use a CPAP machine to get relief. For thousands of people, the answer has been simpler-and quieter-than they ever expected.
Can a mandibular advancement device cure snoring permanently?
No, MADs don’t cure snoring-they manage it. If you stop wearing the device, your jaw returns to its natural position, and snoring typically comes back within 48 hours. It’s a long-term management tool, not a one-time fix. For permanent results, surgical options like UPPP exist, but they carry higher risks and longer recovery times.
Are over-the-counter snoring mouthpieces worth buying?
They’re better than nothing if you can’t afford a custom device, but they’re significantly less effective. Studies show custom MADs reduce snoring by 72% on average, while OTC versions only manage 48%. Many users report jaw pain, poor fit, and inconsistent results. If you’re serious about solving your snoring, investing in a professionally fitted device is worth it.
Do I need a sleep study before getting a MAD?
Yes. Snoring can be a symptom of obstructive sleep apnea, which is a serious medical condition. A sleep study (home or lab-based) is required to rule out moderate-to-severe OSA. If you have severe apnea, a MAD won’t be enough-you’ll likely need CPAP or another treatment. Skipping this step can be dangerous.
How long does it take to get used to wearing a MAD?
Most people adjust within 10-14 days. Initial discomfort-like jaw soreness or excess saliva-is normal. Dentists often recommend wearing the device for short periods during the day to get used to the feeling before using it at night. By day 30, 76% of users are wearing it consistently every night.
Will a MAD damage my teeth or jaw over time?
About 25% of long-term users develop permanent changes to their bite, such as tooth movement or altered jaw alignment. This is why regular dental check-ups every six months are essential. Your dentist will monitor for signs of occlusal changes and can intervene early. Most issues are manageable if caught early, but ignoring them can lead to costly orthodontic work later.
Does insurance cover mandibular advancement devices?
Some do, but not all. In the U.S., only about 38% of private insurance plans cover MADs, and coverage often requires proof of a sleep study and a diagnosis of mild-to-moderate sleep apnea. Medicare rarely covers them unless you have OSA. Check with your provider and ask for a predetermination of benefits before proceeding.
What’s the difference between a MAD and a tongue-retaining device?
MADs move the lower jaw forward to open the airway. Tongue-retaining devices hold the tongue in place using suction to prevent it from falling back. MADs are more common and generally more effective for snoring and mild sleep apnea. Tongue-retaining devices are usually reserved for people who can’t use MADs due to missing teeth or jaw issues, but they’re less comfortable and harder to wear consistently.

Comments
man i tried those otc mouthpieces last year, thought i was gonna finally sleep through the night... turned out i woke up with my jaw locked like a vise and drooled all over my pillow. not worth it. go see a real dentist.
Let me just say - this entire paradigm is a corporate psyop designed by Big Dentistry™ to monetize your sleep deprivation. The FDA doesn't regulate these devices as medical equipment, and the ‘72% efficacy’ stat? That’s from studies funded by SomnoDent. Meanwhile, CPAP - the real gold standard - is being vilified because it’s inconvenient. Wake up. Your airway collapse isn’t a ‘snoring problem’ - it’s a systemic hypoxia crisis masked as a lifestyle tweak. 🤡
i just wanna say i used one of these for 3 years and my husband finally stopped sleeping on the couch. i cried the first night i didn’t wake up to his snoring. also, the jaw pain? yeah, it sucked at first. but now? i forget i’m wearing it. worth every penny. also, i clean mine with vinegar and water. no fancy cleaners needed.
Just wanted to add - if you’re considering a custom MAD, please, please, please get a sleep study first. I didn’t, and I had mild OSA that went undiagnosed for 18 months. The device helped with snoring, but I was still gasping for air at night. My doctor said if I’d waited another year, I might’ve developed hypertension. Don’t be me.
Been using mine for 5 years. No major dental issues. Go to the dentist every 6 months like they said. Clean it. Don’t overthink it. It’s not perfect, but it’s better than sleeping in separate rooms. That’s all I need.
Brothers and sisters - if you snore, you’re not broken. You’re just breathing wrong. This device is not magic. It’s mechanics. Your body is trying to survive the night. The jaw moves forward because evolution didn’t design us for sleeping on our backs with soft tissue collapsing like a deflated balloon. Respect your body. Don’t fight it. Adjust. Adapt. Sleep.
Interesting how this mirrors the historical shift from traditional medicine to patient-centered care. In the 1980s, CPAP was the only option - rigid, authoritarian, imposed. Now we have personalized, biomechanical solutions that empower individuals. This isn’t just a dental device - it’s a cultural evolution in sleep medicine. The fact that adherence is higher speaks volumes about autonomy in treatment.
Of course it works - because you’re all too lazy to just sleep on your side. Why are we medicalizing basic human behavior? People used to sleep on wooden planks and didn’t need $2,000 mouthpieces. Now we’ve turned snoring into a disease so we can sell you more junk. Wake up. You’re not sick - you’re just fat and selfish. And yes, I’m talking to you.
I bought a $60 one off Amazon. Woke up screaming like a banshee because my teeth felt like they were being pulled out by a raccoon. My wife took a photo of my face - I looked like a confused frog who just swallowed a lightbulb. I threw it in the trash. Then I bought a $2,200 custom one. Now I sleep like a baby. And my wife? She kissed me last night. For the first time in 7 years. This isn’t a device - it’s a love potion.
Look - I don’t care if it’s ‘FDA-approved’ or ‘clinically proven.’ This is just another American over-medicalized scam. In my country, we just sleep on our sides and drink turmeric tea. No plastic. No dentists. No $2,000 gadgets. You people are weak. You’ve lost touch with nature. This device? It’s a symbol of your decline.
The human body is a symphony of tension and release. When we sleep supine, gravity becomes the conductor - and the tongue, the viola that falls out of tune. The MAD is not a cure, but a quiet rebellion against entropy. It is not the jaw that moves - but the soul, gently nudging itself toward harmony. To dismiss it as mere plastic is to misunderstand the poetry of anatomy.
bro i got a custom one last year. cost me 1800 but my wife finally stopped yelling at me to stop snoring. the first week was hell - jaw hurt, spit everywhere. now? i forget i have it in. i even take it on trips. the only thing i regret? not doing it sooner. also, dont buy otc ones. they’re garbage. just go to a dentist who knows what they’re doing.
Just wanted to share that my mom got one after her sleep study - she’s 72, has arthritis in her jaw, and still wears it every night. Her dentist adjusted it twice, and now she sleeps through the night without even needing a pillow under her knees. She says it’s the best thing she’s ever done for herself. Honestly? I cried when she told me she hasn’t woken up tired in 6 months. If you’re hesitating - just do it. Your future self will thank you. 💖
Snoring isn’t a joke - it’s a silent cry for help. This device isn’t a luxury. It’s a lifeline. I used to feel guilty for asking my partner to sleep elsewhere. Now? We cuddle. We sleep. We wake up refreshed. No masks. No noise. Just peace. You deserve that. Don’t let fear or cost stop you. Talk to a sleep dentist. Start today. Your future is quieter than you think.