When your liver is under stress-whether from fatty food, alcohol, or metabolic issues-it doesn’t scream. It whispers. By the time symptoms show up, damage may already be advanced. That’s why doctors now rely on noninvasive liver fibrosis tests to catch problems early. Two major tools dominate this space: FibroScan and serum-based scores like FIB-4, APRI, and ELF. Each has strengths, blind spots, and real-world trade-offs you need to understand-not just as a patient, but as someone who wants to take control of their liver health.
How FibroScan Works and What It Measures
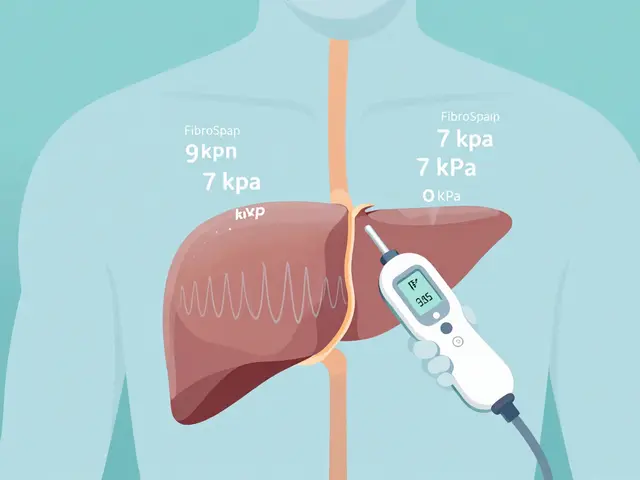
FibroScan is a handheld device that sends a gentle pulse through your skin to measure how stiff your liver is. The stiffer it is, the more scar tissue (fibrosis) is likely present. It uses something called transient elastography, a technology first developed in the late 1990s and commercialized in 2001. Today’s models, like the FibroScan 630, also measure fat buildup in the liver using a metric called CAP (Controlled Attenuation Parameter). Results come out in kilopascals (kPa). A normal liver reads between 2 and 7 kPa. Above 7 kPa? That’s a red flag. Above 12 kPa? That often means advanced fibrosis or cirrhosis. But here’s the catch: FibroScan doesn’t work the same for everyone. If you have a BMI over 28, or if your liver is very fatty (CAP over 268 dB/m), the device might struggle. That’s why the XL probe exists-it’s designed for larger body types. Still, about 10-15% of tests fail to give reliable results, especially in obese patients. The test takes less than five minutes. No needles. No fasting (though you shouldn’t eat within three hours before). You lie on your back, the technician places the probe on your right side, and it does the rest. Results are instant. That’s a big deal. Unlike blood tests that sit in a lab for days, you walk out knowing your liver stiffness right away.Serum Scores: The Blood Test Alternative
Serum scores don’t need a machine. They use routine blood work you’ve probably already had: AST, ALT, platelet count, and sometimes age and glucose. These numbers plug into formulas to estimate fibrosis risk. FIB-4 is the most widely used. It combines age, AST, ALT, and platelets. A score below 1.3 means you’re very unlikely to have advanced fibrosis. A score above 2.67? That’s a high-risk zone. It’s cheap-under $10 to calculate-and built into most electronic health records. Primary care doctors love it because it’s automatic. One study showed using FIB-4 in clinics boosted liver screening from 12% to 67% of at-risk patients. APRI is simpler: just AST and platelets. A score above 2.0 suggests cirrhosis. It’s older and less precise than FIB-4, but still useful in places with limited resources. ELF is more advanced. It measures three specific proteins linked to scarring. It’s not routine, but when FibroScan and FIB-4 disagree, ELF often clears up the confusion. It’s more expensive than FIB-4, but cheaper than a biopsy. The big advantage? These tests need nothing but a blood draw. No special equipment. No training. Just a lab report and a calculator.Accuracy: Who Does Better?
Here’s where things get messy. In controlled studies, FibroScan looks amazing. One 2022 study found it correctly identified cirrhosis with 99% accuracy. But real-world performance? Less impressive. A 2023 study found FibroScan missed nearly half of advanced fibrosis cases (F3/F4). That’s a 54.1% false negative rate. In other words, if your FibroScan says you’re fine, there’s still a more than 50% chance you’re not. FIB-4 isn’t much better at catching advanced disease. It only flagged 16.8% of those same cases. But here’s the twist: FIB-4 is excellent at ruling things out. If your score is under 1.3, there’s a 90% chance you don’t have advanced fibrosis. That’s why experts recommend starting with FIB-4. If it’s low, you’re probably safe. If it’s high, then you move to FibroScan. The real winner? Combining them. A 2020 study showed using FIB-4 first, then FibroScan for borderline cases, cut unnecessary biopsies by 70%. And when you add ELF into the mix for unclear results, accuracy jumps to 85%.
Where the Tests Fall Short
Neither test is perfect. FibroScan can give falsely high readings if you have acute hepatitis, heart failure, or just ate a big meal. It also doesn’t work well in people with very thin or very thick skin. And yes-obesity is a major problem. One Reddit user with a BMI of 38 said his test failed three times before they switched to the XL probe. That added $200 to his bill. FIB-4 has its own issues. It’s unreliable in people under 35. Its accuracy drops from 85% to 67% in younger adults. That’s a problem because NAFLD is rising fast in younger populations. It also can’t distinguish between mild and moderate fibrosis. If your score is 1.8, you’re in a gray zone-neither safe nor clearly at risk. And then there’s CAP, the fat-measuring part of FibroScan. One study found it overpredicted fatty liver by 81% in people with mild fat buildup. So if your CAP says you have 60% fat, you might actually have 30%. That leads to unnecessary worry-and sometimes unnecessary treatment.What Experts Recommend
The European Association for the Study of the Liver (EASL) has a clear protocol: start with FIB-4. If it’s low (<1.3), no further testing needed. If it’s high (>2.67), consider biopsy or FibroScan. If it’s in the middle (1.3-2.67), use FibroScan to clarify. Dr. Brent Tetri from Saint Louis University says it plainly: “No single test should replace clinical judgment.” Your doctor doesn’t just look at numbers. They look at your weight, your alcohol use, your diabetes status, your family history. That context matters. The American Association for the Study of Liver Diseases (AASLD) agrees. Their 2022 guidelines say serum scores are ideal for screening large populations. FibroScan is better for confirming disease in those already flagged. And here’s something new: in 2024, EASL introduced FIB-5, a new serum score that adds glucose levels. It’s especially good for people with diabetes and fatty liver. Early data shows it’s 89% accurate at spotting advanced fibrosis in this group.Cost, Access, and Real-World Barriers
FibroScan costs between $50 and $150 per test. Medicare reimburses about $55. But not every clinic has the machine. You might need to go to a specialty center. That means travel, wait times, and scheduling headaches. FIB-4? It’s already in your lab report. The cost to calculate it? Less than a dollar. That’s why it’s used in rural clinics, community health centers, and even telehealth platforms. But here’s the irony: even though FIB-4 is cheaper and easier, many patients don’t get it. Why? Because doctors don’t always think to order it. Or they assume a normal ALT means a healthy liver. That’s a dangerous assumption. ALT can be normal even with significant fibrosis. A 2023 survey of 1,200 NAFLD patients found 43% were confused by conflicting results. One patient had a FibroScan showing F2 fibrosis but a FIB-4 score suggesting advanced disease. The biopsy that followed confirmed F3. Both tests were wrong in different ways.What Comes Next?
The future is integration. The NIH is testing a three-part algorithm: FIB-4, FibroScan, then ELF if needed. In early trials, it cut unnecessary biopsies by 82% while still catching 94% of cirrhosis cases. Newer FibroScan models, like the 730 released in April 2024, use AI to flag unreliable readings. Early data shows it reduces technical failures by 22%. MRI-based elastography (MRE) is more accurate than FibroScan-but it costs 10 times as much and requires a full MRI machine. It’s not practical for routine screening. Smartphone apps that estimate liver stiffness are being tested, but none have enough validation yet. Don’t trust them.What Should You Do?
If you’re at risk for fatty liver-overweight, diabetic, high cholesterol, or have elevated liver enzymes-ask your doctor for a FIB-4 calculation. It’s free if you’ve had a CBC and liver panel in the last six months. If FIB-4 is borderline or high, ask about FibroScan. If your BMI is over 28, make sure they use the XL probe. If the results conflict, ask about ELF. Don’t rush to biopsy unless the numbers point clearly to advanced disease. And if your doctor says, “Your liver looks fine,” ask: “Did you check my FIB-4?” Most won’t know the answer. That’s your cue to push for better screening. Your liver doesn’t need a biopsy to be understood. It just needs the right tests-and someone who knows how to read them.Is FibroScan better than a liver biopsy?
FibroScan is safer and faster than a biopsy, but it’s not always more accurate. Biopsies still provide the most detailed picture of liver tissue, including inflammation and cell damage. However, FibroScan avoids the risks of bleeding and infection (which occur in about 0.01-0.1% of biopsies) and doesn’t suffer from sampling errors (which affect up to 41% of biopsies). For routine monitoring, FibroScan is preferred. Biopsies are reserved for unclear cases or when other tests disagree.
Can I do a FibroScan at home?
No. FibroScan requires a trained technician and a calibrated device. There are smartphone apps claiming to measure liver stiffness, but none are validated or approved for clinical use. Using them could give you false reassurance or unnecessary panic. Always get FibroScan done in a medical setting.
How often should I get tested for liver fibrosis?
If you have NAFLD or NASH, testing every 1-2 years is recommended. If your FIB-4 is low and you’re making lifestyle changes, you might stretch it to every 3 years. If your score is high or you have diabetes, testing every 6-12 months may be needed. Always follow your doctor’s advice based on your personal risk profile.
What if my FibroScan and FIB-4 give different results?
This happens more often than you’d think. FibroScan can be affected by recent meals, obesity, or inflammation. FIB-4 can be misleading in younger people or those with normal ALT. When results conflict, the next step is usually the ELF test-a blood test that measures three specific fibrosis markers. If ELF still doesn’t clarify, your doctor may recommend a biopsy.
Can I reverse liver fibrosis?
Yes, especially in early stages. Losing 7-10% of your body weight, cutting out alcohol, controlling blood sugar, and managing cholesterol can reduce fibrosis in many people. Studies show that even moderate weight loss can reverse F1-F2 fibrosis. Advanced fibrosis (F3-F4) is harder to reverse, but lifestyle changes still slow progression and reduce the risk of liver failure or cancer.


Comments
This whole post is just corporate fluff disguised as medical advice. FibroScan is a scam designed to make hospitals money. The real solution? Stop eating processed crap and drink water. No device needed.
I had a FibroScan last year and it failed twice because of my BMI. Third time with the XL probe finally worked. Took 10 minutes, zero pain, and I walked out knowing my liver wasn't screaming at me. Honestly? Way better than the blood test that took 3 weeks for results. You don't need a biopsy to feel safe. Just get the right test done. I'm not scared anymore.