Most people don’t realize how much they rely on hearing until it starts slipping away. Maybe you’ve been asking people to repeat themselves, turning up the TV too loud, or struggling to follow conversations in noisy rooms. These aren’t just signs of aging-they could be early warnings of hearing loss. The only way to know for sure is through audiometry testing, the gold standard for measuring how well you hear.
What Exactly Is Audiometry Testing?
Audiometry testing is a simple, non-invasive procedure that checks your ability to hear sounds at different pitches and volumes. It doesn’t hurt. You won’t feel anything more than a slight vibration if bone conduction is used. But the results? They’re powerful. They tell you exactly where your hearing starts to fade-and how much you’re missing. The test measures your hearing threshold: the softest sound you can detect at least half the time. These thresholds are recorded in decibels hearing level (dB HL). Normal hearing is defined as 25 dB HL or better across all tested frequencies. If your threshold is 40 dB HL at 2000 Hz, that means you can’t hear whispers or soft consonants like “s” or “th” unless they’re spoken loudly. The most common type is pure-tone audiometry. You sit in a soundproof booth, wear headphones, and press a button every time you hear a tone. The tones range from low (250 Hz) to high (8000 Hz)-covering the full range of human speech. The audiologist starts with a tone you can easily hear, then lowers the volume in 10 dB steps until you no longer respond. Then they go back up in 5 dB steps to find the exact point where you just barely hear it. This method, called the modified Hughson-Westlake technique, has been used since the 1940s and is still the most accurate way to map hearing loss.Why Air and Bone Conduction Matter
There’s a big difference between hearing a sound through the air and feeling it through your skull. That’s why audiometry tests both air conduction and bone conduction. Air conduction sends sound through your ear canal, eardrum, and middle ear bones before reaching the inner ear. If something’s wrong with your outer or middle ear-like wax buildup, an ear infection, or a perforated eardrum-this path gets blocked. That’s called conductive hearing loss. Bone conduction skips all that. A small oscillator is placed behind your ear on the mastoid bone. It sends vibrations directly to the cochlea, the inner ear’s hearing organ. If your bone conduction thresholds are normal but your air conduction thresholds are worse, you have conductive hearing loss. If both are equally poor, the problem is in your inner ear or auditory nerve-that’s sensorineural hearing loss, the most common type, often caused by aging or noise exposure. The key number? A 15 dB or greater gap between air and bone conduction at any frequency. That’s the official red flag for conductive issues. Without testing both, you’re guessing.Speech Testing: Hearing vs. Understanding
Hearing a tone isn’t the same as understanding a word. That’s why audiometry includes speech testing. Speech Reception Threshold (SRT) testing finds the quietest level at which you can repeat 50% of two-syllable words like “baseball” or “hotdog.” Your SRT should match your average pure-tone threshold at 500, 1000, and 2000 Hz-within ±10 dB. If it doesn’t, something’s off. Maybe the test wasn’t done right. Or maybe you have a hidden problem, like a tumor on the auditory nerve. Then there’s speech discrimination, or word recognition testing. You’ll hear a list of single-syllable words-“cat,” “dog,” “ship”-at a volume 25-40 dB above your threshold. You repeat them. A healthy ear should get 90% or more correct. If you only get 60%, even with amplification, your brain isn’t processing sound properly. That’s common with age-related hearing loss or damage from loud noise. This part is critical. Two people might have the same pure-tone results but wildly different speech understanding. One hears fine in quiet rooms. The other struggles even with hearing aids. Speech testing explains why.Tympanometry: Checking the Middle Ear
Audiometry isn’t just about tones and words. It’s also about pressure. Tympanometry measures how well your eardrum moves. A small probe seals your ear canal and changes the air pressure while playing a low tone. The machine records how much sound bounces back. A healthy eardrum moves freely, letting most sound pass through. If it’s stiff-because of fluid, scar tissue, or a collapsed eardrum-the reading looks flat (Type B tympanogram). That’s a clear sign of middle ear fluid, especially in kids with ear infections. The test takes 3-5 seconds per ear. No discomfort. No noise. Just a quick pressure change. It’s often done alongside pure-tone testing because middle ear problems are one of the most common causes of reversible hearing loss. If you’ve had recurring ear infections or feel like your ears are “plugged,” tympanometry can tell you if it’s just fluid-or something worse.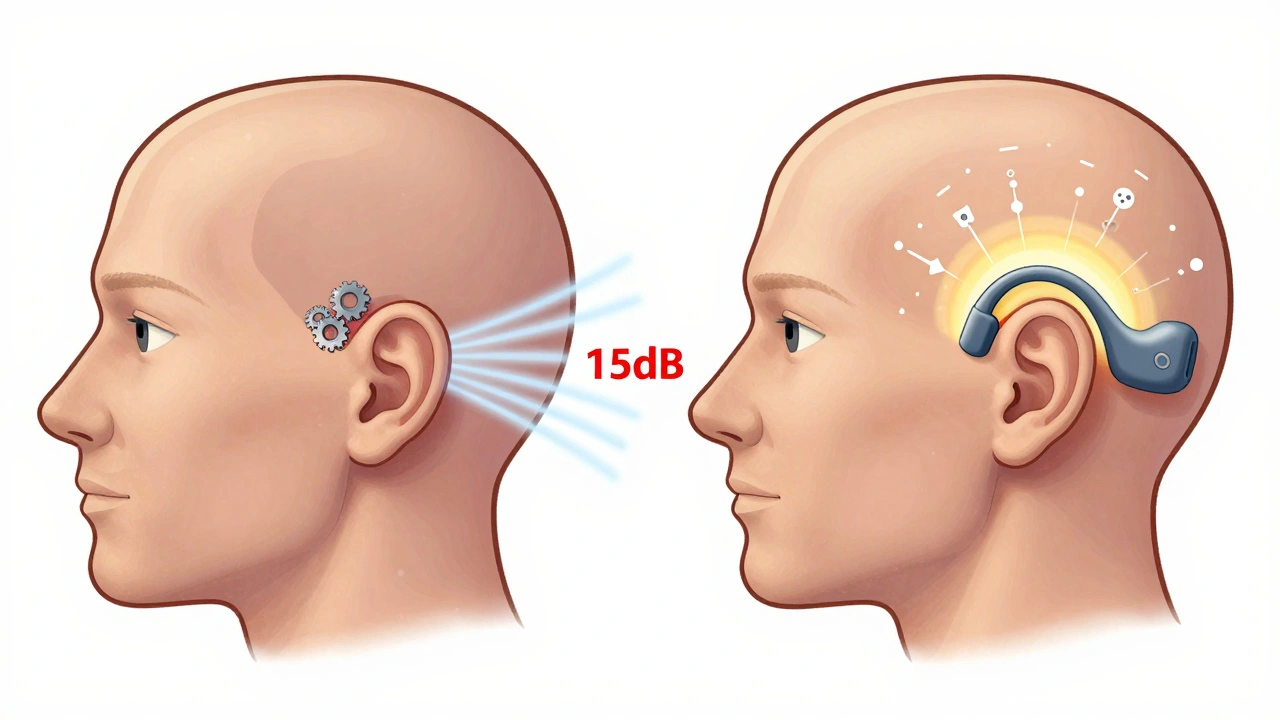
Who Needs Audiometry Testing?
You don’t need to wait until you’re struggling to get tested. Here’s who should have it done:- Anyone over 50-age-related hearing loss starts slowly and often goes unnoticed.
- People exposed to loud noise-construction workers, musicians, factory staff, even frequent concertgoers.
- Those with a family history of hearing loss.
- Patients taking ototoxic medications-like certain antibiotics or chemotherapy drugs (cisplatin).
- Children with delayed speech, frequent ear infections, or who don’t respond when called.
- Newborns-screening is required by law in U.S. hospitals, with diagnostic testing needed by age 3 months if they fail.
What the Results Look Like: Reading Your Audiogram
Your results are shown on an audiogram-a graph with frequency (pitch) on the horizontal axis and decibels (volume) on the vertical axis. Lower numbers mean better hearing. - Circles (○) = Right ear air conduction - Crosses (×) = Left ear air conduction - Brackets ([ ]) = Right ear bone conduction - Less-than signs (<) = Left ear bone conduction A normal audiogram looks like a straight line near the top-below 25 dB across all frequencies. If the dots drop below that, you have hearing loss. The shape tells you the type:- Flat: Equal loss across all pitches
- Sloping: Worse in high frequencies (most common with aging)
- Notched: Dip at 4000 Hz (classic sign of noise damage)
- Reverse slope: Worse in low frequencies (rare, often genetic)
How Accurate Is It? What Can Go Wrong?
Audiometry is highly accurate-when done right. Equipment must be calibrated yearly to ANSI S3.6-2018 standards. If the audiometer is off by even 5 dB, your results are misleading. That’s why reputable clinics check their gear regularly. Patient factors matter too. Fatigue, distraction, or misunderstanding the task can lead to false results. That’s why tests are limited to 45 minutes. If you’re tired, the audiologist will pause or reschedule. Masking is another key step. If one ear is much better than the other, the louder ear might hear the tone meant for the weaker ear. To prevent that, noise is played in the better ear to block it out. Skip masking, and you get inaccurate thresholds. About 12% of tests have masking errors, according to Mayo Clinic data.
What Comes After the Test?
Audiometry doesn’t end with the graph. The real value is in what happens next. If you have hearing loss, your audiologist will explain:- What type you have
- How severe it is (mild, moderate, severe, profound)
- Whether it’s treatable
- What hearing aids or assistive devices might help
- If you need a referral to an ENT doctor
Tele-Audiology and New Tech
You don’t always need to go to a clinic anymore. Since the pandemic, tele-audiology has grown. The FDA now approves remote testing using devices like the KUDUwave mobile booth. You can do a basic hearing screen at home with a smartphone app or tablet. But here’s the catch: these tools aren’t reliable for detecting mild hearing loss below 25 dB HL. They’re great for screening, but not for diagnosis. New AI tools are starting to help audiologists interpret audiograms faster. Otometrics’ AI software, for example, identifies conductive loss patterns with 92% accuracy in trials. But it’s still a tool-human expertise is irreplaceable.Where to Get Tested
You can find audiometry testing at:- ENT clinics
- Dedicated audiology practices
- Hospitals
- Some retail hearing centers (for screening only)
Final Thoughts: Don’t Wait Until It’s Too Late
Hearing loss doesn’t come with a siren. It creeps in slowly. You adapt. You think you’re fine. But every missed conversation, every misunderstood word, adds up. Audiometry testing takes less than an hour. It’s painless. It’s accurate. And it gives you back control. Whether you’re 25 and work in a noisy warehouse or 70 and can’t hear your grandchildren, knowing your hearing status is the first step to fixing it. Don’t wait for someone to tell you to get tested. If you’ve noticed any change in your hearing-ask for an audiometry test. It’s not just about volume. It’s about connection.Is audiometry testing painful?
No, audiometry testing is completely painless. You’ll hear tones through headphones or feel a slight vibration if bone conduction is used. There are no needles, no probes inside your ear, and no discomfort. Some people find the bone oscillator slightly uncomfortable if they wear glasses, but it’s brief and not harmful.
How long does an audiometry test take?
A full diagnostic audiometry test usually takes 30 to 45 minutes. This includes air and bone conduction testing, speech recognition, and tympanometry. Screening tests, like those done at pharmacies or schools, can be done in under 10 minutes but don’t provide the full picture.
Can I do audiometry testing at home?
You can do basic hearing screenings at home using smartphone apps or online tools, but they’re not reliable for diagnosis. These tools can’t accurately measure thresholds below 25 dB HL and can’t perform bone conduction or masking. For accurate results, you need a certified audiologist using calibrated equipment in a soundproof room.
What does 25 dB HL mean?
25 dB HL is the upper limit of normal hearing. It means you can hear sounds as soft as a whisper at a distance of about 6 feet. If your threshold is 30 dB HL or higher, you have mild hearing loss-you might miss soft speech, especially in noisy places. The lower the number, the better your hearing.
Why do I need speech testing if I already had tone testing?
Tone testing tells you how loud sounds need to be. Speech testing tells you how well your brain understands them. Two people might hear the same tones but one struggles to understand words. That’s because hearing and understanding are different processes. Speech testing helps determine if hearing aids will help you communicate-or if there’s a deeper neurological issue.
How often should I get my hearing tested?
If you’re over 50, get tested every 2-3 years. If you’re exposed to loud noise regularly, get tested annually. If you’ve been diagnosed with hearing loss, follow your audiologist’s recommendation-usually every year to track changes. For children with hearing loss or risk factors, testing may be needed every 6 months.



Comments
Just got my audiogram back last week-turns out I’ve been hearing like I’m underwater in a swimming pool. Turns out my high frequencies are toast. No wonder my dog hears the fridge door before I do. 😅
Let me guess-you’re one of those people who think hearing loss is just ‘getting old.’ Nope. It’s the sound of your brain slowly giving up on decoding the world. I used to work in a factory where they played AC/DC at 110 dB for 8 hours a day. My audiogram looks like a mountain range after an earthquake. And yeah, I still listen to Metallica. Just with earplugs now. You don’t lose your soul to loud music-you lose your ability to hear your own damn thoughts. 🤘
My grandmother refused to get tested for years-said, ‘If I can’t hear the TV, I can just turn it up!’ Then one day she missed my father’s heart attack because she didn’t hear him call for help. Now she wears hearing aids and cries every time she hears birds again. Hearing isn’t just about sound-it’s about connection. And we lose so much before we even notice it’s gone.
Okay, but let’s be real-most people don’t get tested because they’re scared of what they’ll find. I’m a nurse, and I’ve seen it a hundred times: people come in with 70 dB loss, claim they ‘just need louder TV,’ and then act like it’s the audiologist’s fault they didn’t notice their kid calling them from the other room for three years. It’s not aging-it’s denial. And if you’re over 40 and haven’t had a baseline test? You’re playing Russian roulette with your brain. Get it done. Your future self will thank you. Also, earplugs at concerts. Yes, even if you’re ‘that guy.’
This post is just a marketing pamphlet for audiologists. Everyone knows hearing loss is inevitable. You’re not ‘saving’ anyone by making them sit in a soundproof box and press buttons. People die of cancer, starvation, war-yet you want me to care about whether I can hear a 4000 Hz tone? Pathetic. Your whole industry profits off fear. Go fix the world’s real problems before you sell me a $300 hearing aid.
There’s a grammatical error in the post: ‘It doesn’t hurt. You won’t feel anything more than a slight vibration if bone conduction is used. But the results? They’re powerful.’ The second sentence is a fragment. Also, ‘less-than signs (’ is cut off. Minor, but still. If you’re going to write a technical piece, at least proofread.
As someone who spent years teaching deaf children to lip-read, I can tell you that hearing loss isn’t a medical footnote-it’s a linguistic and emotional earthquake. When a child can’t hear their mother’s voice for the first time, it reshapes their entire relationship with language. And when an adult loses their ability to hear laughter, the silence is heavier than any decibel chart can quantify. Audiometry isn’t just about numbers-it’s about reclaiming the poetry of everyday sound: the rustle of pages, the hum of a kettle, the way your partner sighs when they’re tired. We don’t test hearing to measure loss-we test it to measure what’s still worth saving.
Hey, I’m a musician and I’ve been using custom earplugs for gigs since 2018. Honestly, it changed my life. I can hear the music better now-cleaner, clearer, no ringing. People think earplugs dull sound, but nope. It’s like turning down the bass on a bad speaker. You actually hear the details. Also, if you’re reading this and you’re over 30 and go to concerts? Get custom molds. They’re expensive, but cheaper than hearing aids. And yes, I’m totally preaching to the choir here-but I’m happy to preach.
Wow. I didn’t expect a philosopher and a nurse to drop truth bombs in the same thread. And now a musician? This is why I love Reddit. You people turn a clinical topic into a damn symphony of lived experience. I’m gonna go get my ears checked tomorrow. Not because I’m scared. Because I want to hear my daughter say ‘I love you’ without asking her to repeat it.