Metformin Contrast Dye Risk Calculator
Risk Assessment Tool
This calculator helps determine whether you should continue taking metformin before a medical imaging procedure involving contrast dye.
Recommendation
Every year, millions of people with type 2 diabetes get an imaging scan-whether it’s a CT scan for abdominal pain, a coronary angiogram for chest discomfort, or a kidney ultrasound for unexplained swelling. And every time, there’s a question that pops up: Should I stop my metformin before the contrast dye? For years, the answer was a hard yes. But today, that’s no longer the rule. The truth is more nuanced, and getting it wrong can hurt more than help.
Why the Fear of Lactic Acidosis Exists
Metformin has been the go-to pill for type 2 diabetes since the mid-90s. It’s cheap, effective, and doesn’t cause weight gain or low blood sugar. But it’s also cleared by the kidneys. When kidney function drops, metformin can build up. And when metformin builds up, it can interfere with how your cells use oxygen. That’s where lactic acidosis comes in. Lactic acidosis isn’t just high lactate-it’s a dangerous drop in blood pH. It happens when your body shifts from burning sugar with oxygen (aerobic) to burning it without oxygen (anaerobic). Metformin makes this shift more likely by blocking a key step in cellular energy production. The result? Lactate piles up, your blood turns acidic, and your organs start to fail. The scary part? About 40% of people who develop metformin-associated lactic acidosis (MALA) don’t survive. But here’s the twist: this almost never happens in healthy people.Contrast Dye Isn’t the Enemy-Kidney Trouble Is
Iodinated contrast dye, used in CT scans and angiograms, can temporarily reduce kidney function. This is called contrast-induced acute kidney injury (CI-AKI). In some people, especially those over 65 or with existing kidney disease, the kidneys slow down for a day or two after the scan. That’s when metformin might not get flushed out fast enough. But here’s what most people don’t realize: contrast dye doesn’t cause lactic acidosis. It only creates a window where metformin might accumulate-if your kidneys were already struggling. If your kidneys are working fine, even a strong dose of contrast won’t trigger this. Studies show that fewer than 10 cases of MALA happen per 100,000 patient-years of metformin use. That’s rarer than being struck by lightning. And in patients with normal kidney function, the risk of lactic acidosis after contrast dye is practically zero.What Changed in 2016? (And Why It Matters)
Before 2016, the FDA told doctors to stop metformin before any procedure involving contrast dye-no exceptions. Patients would go off their diabetes meds for 48 hours, sometimes longer. That meant blood sugar spikes, hospital visits, and even diabetic ketoacidosis in some cases. Then came the evidence. Large studies showed that patients with normal kidney function (eGFR above 60 mL/min/1.73 m²) had no increased risk of lactic acidosis after IV contrast. The FDA updated its label. The American College of Radiology and National Kidney Foundation followed. Now, the rules are clear:- If your eGFR is above 60 and you have no other risk factors-you can keep taking metformin. No pause. No worry.
- If your eGFR is between 30 and 60, or you have heart failure, liver disease, or are over 65-you should hold metformin at the time of the scan.
- If you’re getting contrast through an artery (like in a heart catheterization)-stop metformin regardless of kidney function.
Who’s at Real Risk?
Not everyone with diabetes needs to stop metformin. But some people do. Here’s who should be cautious:- eGFR between 30 and 60 mL/min/1.73 m²
- Heart failure (especially recent or unstable)
- Severe liver disease
- History of alcohol abuse
- Age 65 or older with other health issues
- Dehydration or infection at the time of the scan
- Receiving contrast directly into an artery (IA)
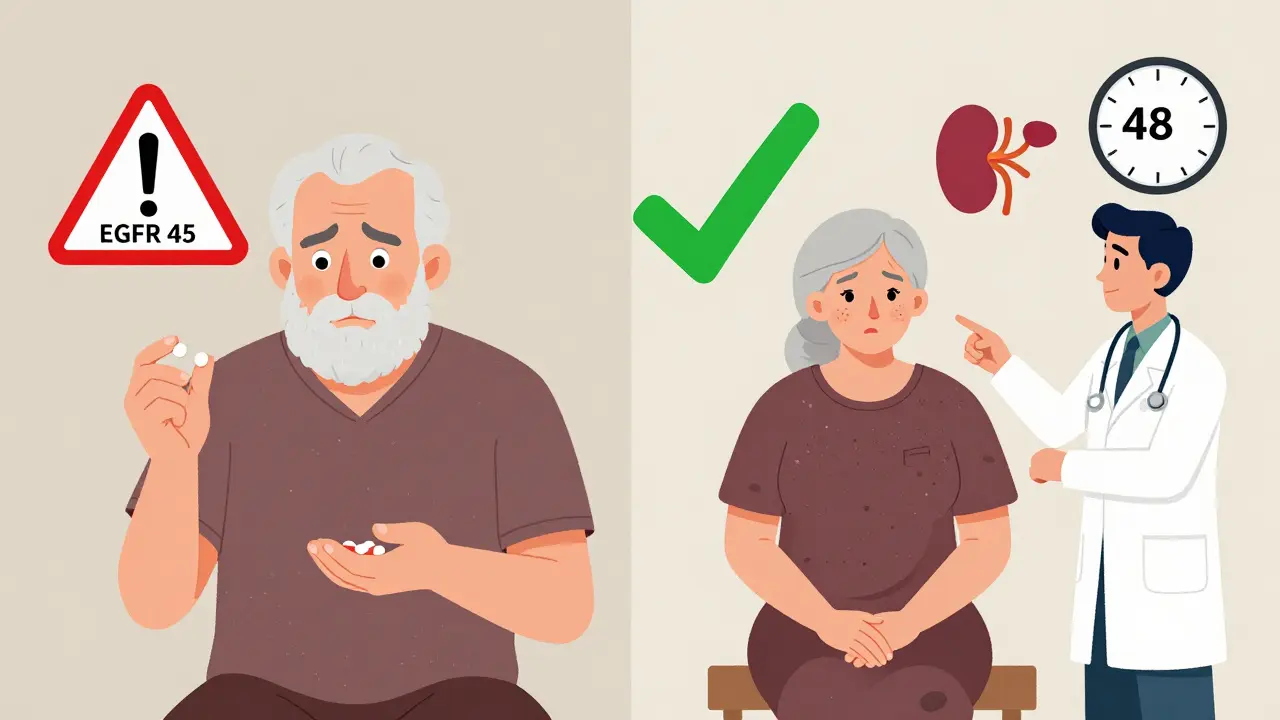
What Happens After the Scan?
If you stopped metformin, you don’t just restart it the next day. You wait 48 hours-and get your kidney function checked again. Why? Because if your kidneys didn’t bounce back, restarting metformin could still be dangerous. A simple blood test-creatinine and eGFR-is all it takes. If your numbers are back to normal, you can safely resume your dose. If your kidney function is still low, your doctor might delay restarting metformin or switch you to another medication temporarily. Insulin, SGLT2 inhibitors, or GLP-1 agonists are common alternatives.What About Dialysis?
If you’re on dialysis, you’re already managing kidney failure. Metformin is usually avoided in advanced kidney disease-but if you’re on it, your care team knows the drill. For patients on intermittent hemodialysis, metformin is typically held before the procedure and restarted after dialysis, since dialysis clears both metformin and lactate. For those on continuous dialysis (CRRT), metformin clearance drops to about 50 mL/min, so timing matters even more.What If You Already Took Metformin Before the Scan?
If you accidentally took your metformin right before your scan and your eGFR is normal-don’t panic. There’s no evidence this leads to lactic acidosis. If your kidney function is borderline (eGFR 40-60), monitor for symptoms: nausea, vomiting, deep breathing, confusion, muscle weakness, or unusual fatigue. If any appear, get to an ER. Lactic acidosis is rare, but it’s serious. Blood tests for lactate and pH can confirm it quickly.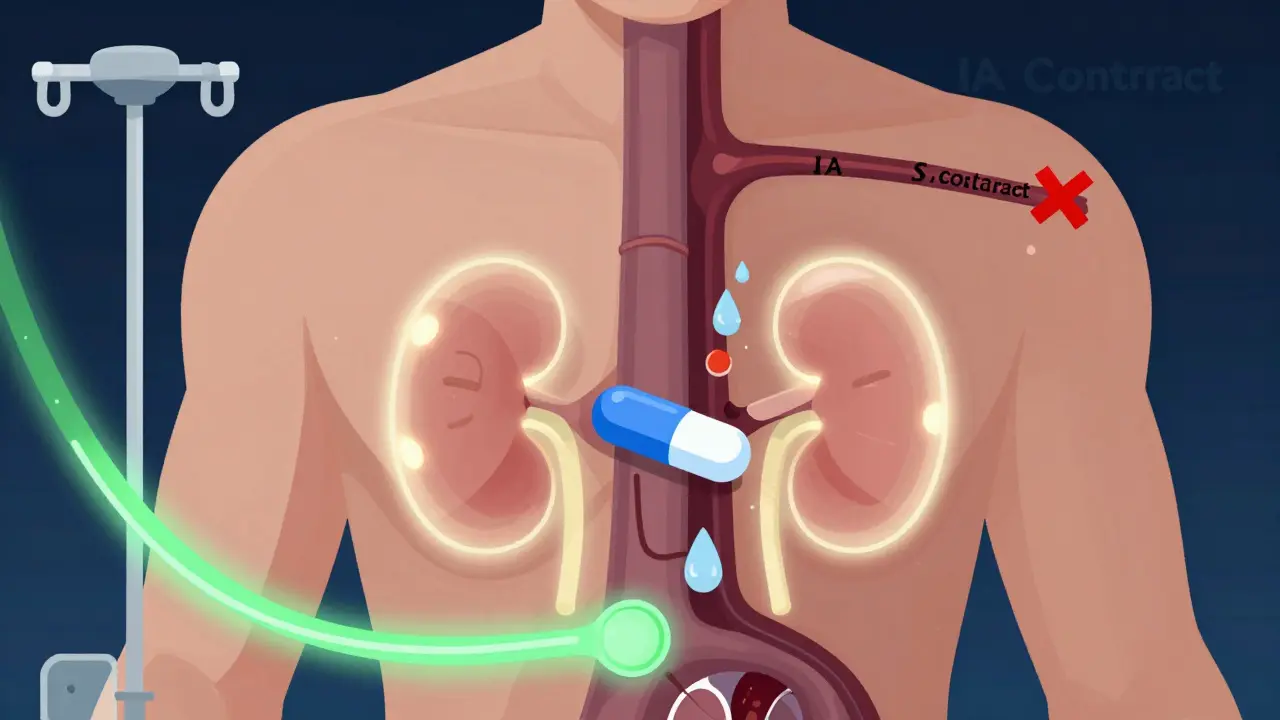
Why This Matters Beyond the Scan
Stopping metformin unnecessarily isn’t harmless. It leads to high blood sugar for days. That’s stressful on your heart, your kidneys, and your blood vessels. For many, it means emergency visits, insulin injections, or even hospitalization. The shift in guidelines reflects a bigger trend: medicine is moving away from blanket rules and toward smart, individualized care. We’re learning that the risk of stopping metformin often outweighs the risk of keeping it-when done right.What’s Next?
Researchers are now looking at genetic factors that might make some people more prone to lactic acidosis. Could a simple DNA test someday tell you if you’re at higher risk? Maybe. For now, the best approach is simple:- Know your eGFR. Ask for it at your next blood test.
- Don’t assume you need to stop metformin. Ask your doctor if you qualify for an exception.
- If you’re told to hold it, ask when to restart-and insist on a follow-up kidney check.
- If you’re on contrast dye and feel unwell afterward, speak up. Lactic acidosis is rare, but early treatment saves lives.
Frequently Asked Questions
Can I take metformin after a CT scan with contrast dye?
Yes-if your kidney function is normal (eGFR above 60 mL/min/1.73 m²) and you’re not getting contrast through an artery. If your eGFR is between 30 and 60, or you have heart failure, liver disease, or are over 65, you should wait 48 hours and get your kidney function checked before restarting.
Is lactic acidosis common with metformin and contrast dye?
No. Fewer than 10 cases occur per 100,000 patients per year. Most cases happen in people with multiple risk factors-like kidney failure, heart failure, or infection-not in healthy individuals getting a routine CT scan.
What’s the difference between IV and arterial contrast?
Intravenous (IV) contrast is injected into a vein, like for a standard CT scan. Arterial (IA) contrast is injected directly into an artery, like during a heart catheterization. IA contrast carries a higher risk of kidney stress, so metformin must be stopped regardless of kidney function.
Should I stop metformin if I’m dehydrated before a scan?
Yes. Dehydration stresses your kidneys and increases the chance of contrast-induced injury. If you’re dehydrated, hold metformin and reschedule the scan once you’re well-hydrated. Drink water the day before and avoid alcohol or caffeine.
Can metformin cause kidney damage?
No. Metformin doesn’t damage kidneys. But it’s cleared by them. If your kidneys are already failing, metformin can build up and raise your risk of lactic acidosis. That’s why it’s avoided in advanced kidney disease-not because it harms the kidneys, but because your body can’t clear it safely.
What are the signs of lactic acidosis?
Symptoms include nausea, vomiting, stomach pain, unusual tiredness, dizziness, rapid breathing, muscle cramps, and feeling cold. If you have these after a scan and are on metformin, seek emergency care. Blood tests will confirm high lactate and low pH.
How long does metformin stay in the body?
In healthy kidneys, metformin’s half-life is 6-9 hours. About 90% is cleared in 24 hours. But if your kidneys are impaired, it can linger for days. That’s why checking kidney function before restarting is so important.



Comments
Just had my CT last week and was so relieved to see this info-my doctor told me to keep taking metformin, and I was terrified I’d mess up my kidneys. Turns out I’m fine. Thank you for clarifying this so clearly.
I appreciate how this breaks down the real risks without fearmongering. Too many providers still default to stopping metformin out of habit, not evidence. Patients deserve better than blanket protocols.
As someone who grew up in a country where diabetes meds are rationed and scans are rare, it’s wild to see how nuanced our protocols have become. This is precision medicine at its best-no more one-size-fits-all.
Let’s be real-this whole ‘safe to continue’ thing is just Big Pharma spinning the data. They don’t want you to stop metformin because it’s cheap. The real risk? It’s buried in the footnotes. You think they’d tell you if the FDA knew about the 2003 study where 3 patients died after contrast? No way.
I’m so glad someone finally explained this without jargon-my mom, who’s 72 and has mild kidney issues, was about to refuse her CT because she was told to stop metformin. Now I’ve printed this out and handed it to her doctor. Thank you for writing this.
Ah, the grand epistemological paradox of modern medicine: we quantify risk with eGFR, yet we still treat the patient as a statistical outlier rather than a sentient being navigating a system built on probabilistic approximations. The real tragedy isn’t lactic acidosis-it’s the erosion of clinical intuition in favor of algorithmic dogma.
You people act like this is new news but I been telling my cousin who works in hospital since 2018 that they stop metformin too much. People get scared and do what they think is safe but its worse. My cousin say they get more diabetic emergencies from stopping metformin than from contrast. You think the hospital wants to deal with ketoacidosis? No they want to do the scan and go home. So they stop the pill and then the patient comes back sick. This is why I say doctors are lazy.
There’s a deeper layer here that rarely gets discussed: the psychological burden of being told to stop a medication you’ve taken daily for years. It’s not just about physiology-it’s about identity. Metformin becomes part of your routine, your sense of control. When you’re told to stop it, even for 48 hours, it feels like your body is betraying you. The fear isn’t just of lactic acidosis-it’s of losing autonomy over your own health. That’s why the shift in guidelines matters more than the numbers: it restores trust.
Guidelines updated. Evidence supports. No change needed.
Finally someone says it right. Stop overcomplicating. If your kidneys are good keep taking it. If they’re not stop it. Done. Stop making people panic over a 0.01% risk.
My nurse practitioner showed me this exact chart last week. I was about to cancel my CT because I was scared. Now I’m just glad I didn’t listen to the random Reddit advice that said ‘never take metformin near contrast.’ Honestly? This post saved me a lot of stress.
Just got my eGFR back-62! So I kept my metformin for the CT and felt so proud of myself for asking questions instead of just following orders. Also my cat sat on my lap the whole time I waited for results. Best therapy.
One thing I’d add: hydration matters more than people realize. Drinking water before and after the scan isn’t just ‘good advice’-it’s the most effective way to protect your kidneys. Simple, free, and often overlooked.
I’m curious-has anyone seen data on how often patients actually get their kidney function checked after restarting metformin? I’ve heard stories of people just resuming it without a follow-up. Is that common enough to warrant a system change?
It’s fascinating how the medical community’s response to this issue mirrors broader societal trends: we’ve moved from rigid, top-down protocols to individualized risk assessment. This isn’t just about metformin-it’s about the evolution of medical paternalism into patient-centered care. The fact that we now trust patients to understand eGFR values, to ask about IV vs. IA contrast, to advocate for follow-up labs-this represents a quiet revolution in healthcare. The real victory isn’t the lowered incidence of lactic acidosis; it’s that patients are now active participants in their own safety. And that shift? That’s the real breakthrough.