When you hear the word generic, you probably think of cheap pills that work just like the brand name. But when it comes to biologics, that’s not the whole story. Biologics aren’t made in a lab like aspirin or metformin. They’re made from living cells - think proteins, antibodies, or complex molecules grown in bioreactors. That’s why you can’t just copy them exactly. Instead, you get something called a biosimilar.
What’s the real price difference?
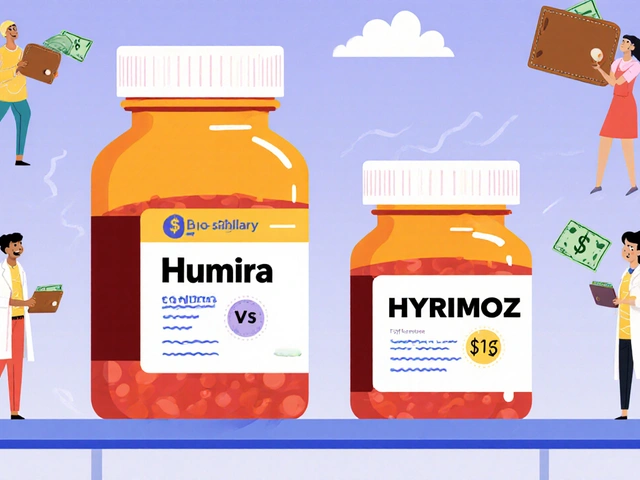
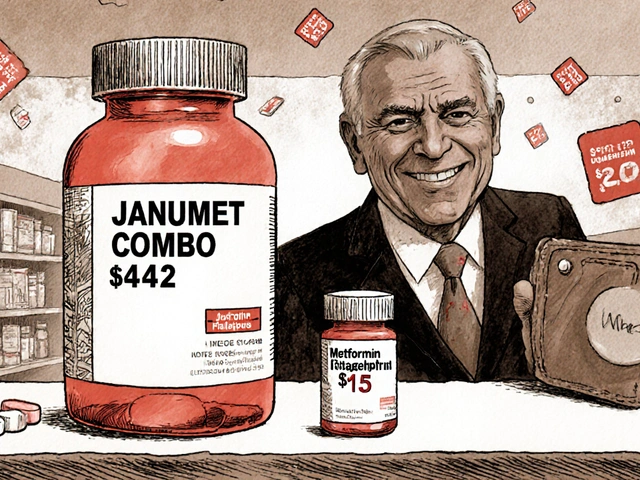
In 2025, the average 30-day prescription for a brand biologic in the U.S. costs $2,104. The biosimilar version? $919. That’s more than half off - a 56.3% drop. For patients paying out of pocket, that means saving nearly $300 a month. Over a year, that’s over $3,600 in savings per person. Take Humira, for example. Before biosimilars hit the market, it cost about $80,000 per patient per year. Now, with biosimilars like Hyrimoz and Amjevita, the price has dropped by 80%. Sixty-five percent of new prescriptions for adalimumab are now biosimilars. That’s not a small shift - it’s a market revolution. But here’s the catch: not all biosimilars are priced the same. The first ones to launch often offer the biggest discounts - sometimes 50% to 80% off. As more competitors enter, prices keep falling. Meanwhile, the original brand drug doesn’t just sit still. In fact, brand biologics have lowered their prices by an average of 25% just to stay competitive after a biosimilar enters the market. That’s rare in pharma - usually, brands raise prices, not cut them.Why aren’t biosimilars everywhere?
You’d think with savings this big, everyone would switch. But they don’t. Only about 15-20% of biologics in the U.S. are biosimilars today. Compare that to traditional generics - they make up 90% of all prescriptions but cost only 13% of total drug spending. Why the gap? One reason is patents. Brand companies don’t just rely on one patent. They file dozens - sometimes over a hundred - covering everything from manufacturing methods to delivery devices. These are called “patent thickets.” They delay biosimilar entry by years. One study found that for every biologic that loses its main patent, there are still 3-5 secondary patents blocking competitors. Then there’s the role of Pharmacy Benefit Managers (PBMs). These are the middlemen who negotiate drug prices for insurers. But here’s the twist: PBMs often get bigger rebates from brand biologics than from biosimilars. So even though biosimilars are cheaper, insurers may still prefer the brand because the PBM gets paid more to push it. It’s a system that rewards high prices, not low ones. Doctors and patients also get confused. Many still think biosimilars are “less effective” or “not as good.” But the FDA says they’re not. Every approved biosimilar has been tested in clinical trials and shown to work just like the original. No difference in safety. No difference in how well it works. The FDA has approved 76 biosimilars as of October 2025 - and none have been pulled for safety issues.How much have biosimilars saved so far?
The numbers are staggering. Since 2015, biosimilars have saved the U.S. healthcare system between $36 billion and $56 billion, depending on who’s counting. In 2024 alone, savings hit $12.4 billion to $20 billion. That’s enough to cover the cost of care for hundreds of thousands of patients with rheumatoid arthritis, Crohn’s disease, or cancer. The Association for Accessible Medicines estimates that if biosimilars reached 40% market share by 2030, they could save $125 billion annually. That’s not a guess - it’s based on real-world data from Europe, where biosimilars are used more widely. In countries like Germany and Sweden, biosimilar adoption is over 70% for some drugs. And those countries pay far less for biologics than the U.S. does.
What’s blocking the next wave of savings?
The biggest barrier isn’t science. It’s money - and who controls it. Developing a biosimilar costs between $100 million and $250 million. That’s a lot, but it’s still far less than the $2 billion it takes to develop a new biologic. Still, few companies take the risk because the payoff isn’t guaranteed. If a brand company pushes back with legal battles or rebate deals, the biosimilar maker could lose money. The Inflation Reduction Act added another layer of complexity. It now requires drugmakers to pay rebates to Medicare if prices rise faster than inflation. But the law doesn’t clearly say whether biosimilars count as “new drugs” or “existing drugs.” That uncertainty makes it harder for manufacturers to plan long-term. And then there’s the FDA. While they’ve approved 76 biosimilars, only about 10% of the biologics expected to lose patent protection in the next 10 years even have a biosimilar in development. Why? Because the approval process is still slow and expensive. The FDA is trying to fix that. In September 2025, they released new draft guidance to simplify testing and reduce the need for redundant clinical trials. That could cut development time by 1-2 years.What’s next?
The future of biosimilars isn’t just about saving money - it’s about making life-saving treatments accessible. Right now, many patients skip doses or stop treatment because they can’t afford the brand biologic. A 2024 study found that 1 in 5 patients with autoimmune diseases cut back on their biologic because of cost. That leads to worse outcomes, more hospital visits, and higher long-term costs. If we fix the system - remove patent thickets, align PBM incentives, simplify approvals - we could save over $42 billion in medical costs by 2027, according to the Department of Health and Human Services. That’s not just a number. It’s more insulin for diabetics, more cancer drugs for patients, more treatments for people who need them. The technology is ready. The science is proven. The savings are real. What’s missing is the will to change how we pay for medicine.
What patients should know
If you’re on a brand biologic, ask your doctor: “Is there a biosimilar version available?” If your insurance won’t cover it, ask them to appeal. Many insurers cover biosimilars at lower copays - sometimes as low as $10 a month. If you’re on Medicare, check if your Part D plan includes biosimilars. They’re often in Tier 2, not Tier 3 or 4. Don’t assume your drug has no cheaper option. Even if your prescription says “Humira,” there may be six biosimilars approved for it. Your doctor might not know. But you can ask.What insurers and employers should know
Switching to biosimilars isn’t just ethical - it’s smart business. For every 10% increase in biosimilar use, drug spending drops by 5-7%. That’s not a small dent. For a company with 10,000 employees, shifting just 30% of biologic prescriptions to biosimilars could save $1.5 million a year. And it’s not just about cost. Better access means fewer disability claims, fewer missed workdays, and lower long-term healthcare costs. The ROI is clear.Are biosimilars the same as generic drugs?
No. Generic drugs are exact chemical copies of small-molecule drugs like statins or antibiotics. Biosimilars are highly similar but not identical to complex biologic drugs made from living cells. They can’t be exact copies because their structure is too complex. But they work the same way and are proven to be just as safe and effective.
Why are biosimilars cheaper if they’re so complex?
Because they don’t need to repeat the full clinical trials that the original brand did. The brand company spent billions developing the drug and proving it works. A biosimilar maker only needs to show it’s highly similar and works the same way - which costs $100-250 million instead of $2 billion. That’s why they can be priced 40-80% lower.
Do biosimilars work as well as brand biologics?
Yes. Every FDA-approved biosimilar has been tested in clinical trials against the original drug. Studies show no meaningful difference in how well they work or their safety profile. The FDA requires this before approval. Thousands of patients have switched from brand to biosimilar with no loss of effectiveness.
Why don’t doctors prescribe biosimilars more often?
Many doctors aren’t trained on biosimilars or aren’t aware of the latest options. Some still believe biosimilars are inferior - even though the science says otherwise. Others are influenced by pharmaceutical reps who push brand drugs. And in some cases, insurance rules or rebate structures make it harder to switch.
Can I switch from a brand biologic to a biosimilar safely?
Yes. The FDA and major medical societies support switching. Studies show patients who switch from brand to biosimilar maintain the same level of disease control. Some patients even report fewer side effects, possibly because the biosimilar is manufactured differently. Always talk to your doctor before switching, but there’s no medical reason to avoid it.
Will biosimilar prices keep falling?
Yes - if more companies enter the market. The first biosimilar for a drug often offers the biggest discount. As more biosimilars launch, prices drop further. For example, after five biosimilars entered the adalimumab market, the average price fell by 80%. That’s what happens when competition kicks in.
Are biosimilars covered by insurance?
Most major insurers and Medicare Part D plans cover biosimilars - often at lower copays than the brand. Some plans require you to try the biosimilar first. Others cover both but charge a higher copay for the brand. Check your plan’s formulary or call your insurer. Don’t assume you’re stuck paying full price.


Comments
So let me get this straight - we’ve got drugs that cost $80k a year, and now we can get the same thing for $16k? And people still argue about it? This isn’t healthcare, it’s a casino where the house always wins.
Wait so biosimilars are cheaper but not exact copies? So like… they’re kinda the same but not? That’s wild.
I’ve been on Humira for 8 years. My copay was $450/month until my biosimilar switched last year. Now it’s $12. I cried in the pharmacy. No one talks about this enough.
Why does my doctor still push the brand? I asked about biosimilars and he just said ‘we’ll stick with what works.’ But what works costs 5x more. That’s not medicine, that’s inertia.
Let me break this down logically, because this is a systemic failure that requires multi-layered analysis. In the U.S., pharmaceutical pricing is not governed by cost of production but by market power and regulatory capture. PBMs are not neutral intermediaries - they are profit-maximizing entities incentivized to promote higher-priced drugs through rebate structures that distort formularies. This creates a perverse outcome where the cheapest, safest, and most clinically equivalent option is systematically suppressed. The patent thicket strategy - filing dozens of secondary patents on delivery mechanisms, packaging, or minor formulation tweaks - is a legal loophole that extends monopolies beyond the original 20-year window. This is not innovation, it’s rent-seeking dressed up as intellectual property protection. Meanwhile, the FDA’s approval process, while rigorous, remains unnecessarily burdensome for biosimilars due to legacy requirements that were designed for small-molecule generics. The $100–250 million development cost is a barrier not because of science, but because of litigation risk. If a brand company sues you into bankruptcy before you even launch, what investor will touch this space? And now, with the Inflation Reduction Act’s ambiguity around whether biosimilars count as ‘new’ or ‘existing’ drugs, the regulatory fog has thickened further. This is not a drug access problem - it’s a capitalism problem. We’ve outsourced healthcare to shareholders and lobbyists, and patients are paying the price - literally, with their lives.
Thank you for sharing this comprehensive overview. As someone who works in health policy, I can confirm that the data you’ve presented aligns with peer-reviewed studies from JAMA and Health Affairs. The 56.3% price drop for biosimilars is consistent with CMS estimates, and the 80% reduction for adalimumab is well-documented. However, adoption remains low not due to clinical uncertainty - the FDA’s 76 approvals and zero safety withdrawals speak for themselves - but because of structural misalignments in reimbursement. Insurers often favor brand drugs because PBMs receive higher rebates, creating a hidden financial incentive to maintain high prices. This is a classic principal-agent problem: the payer (insurer) is supposed to act in the patient’s interest, but is instead incentivized by the middleman’s rebate structure. The solution lies in transparency: requiring PBMs to pass rebates directly to consumers, eliminating anti-competitive patent strategies, and mandating provider education on biosimilar equivalence. This isn’t theoretical - Germany achieves 70% adoption because they’ve done exactly this. We can, too.
Wait - so… you’re saying… that the entire U.S. pharmaceutical system… is… rigged?!!? By… patent thickets… and… PBM rebates… and… FDA ambiguity… and… doctor ignorance… and… insurance disincentives… and… investor fear… and… regulatory inertia… and… corporate greed… and… systemic failure… and… human apathy… and… economic irrationality…?!?! And you think… we can fix this… with… policy…?!?! You’re either a visionary… or… you’ve been drinking the Kool-Aid… from the same vat… that the FDA… and… the AMA… and… the Big Pharma lobbyists… all… stirred… together… with… a… spoon… made… of… lies… and… tax write-offs…
Actually, you're all missing the real issue. Biosimilars aren't even approved in the EU the same way as in the U.S. The EMA requires more analytical data, and even then, switching isn't always recommended for chronic patients. Plus, the 80% price drop you mention? That's only in the first year. After that, prices stabilize. And let's not forget - biosimilars still need cold chain storage, which adds cost. Also, the FDA's 76 approvals include some that never even launched. Real market penetration is lower than the numbers suggest. You're oversimplifying a complex regulatory and logistical landscape.