CHF Fluid Management Calculator
Imagine waking up with swollen ankles, a tight chest, and a scale that seems to climb overnight. For many living with Congestive Heart Failure - a condition where the heart can’t pump blood efficiently - those mornings are a painful reminder of fluid retention. Managing it isn’t just about taking pills; it’s a daily dance of diet, medication, and self‑monitoring. Below you’ll find a step‑by‑step playbook to keep the excess fluid at bay and improve quality of life.
What Causes Fluid Retention in CHF?
When the heart’s pumping power drops, blood backs up in the veins. The kidneys sense lower blood flow and respond by holding onto sodium and water - a survival instinct that backfires in Congestive Heart Failure. The result is swelling (edema), weight gain, and shortness of breath. Understanding this loop helps you break it.
Assessing the Severity
- Look for peripheral edema: puffiness in ankles, calves, or abdomen.
- Track shortness of breath, especially when lying flat (orthopnea).
- Use the NYHA (New York Heart Association) classification to gauge functional limitation - Class II means slight limitation, Class IV means symptoms at rest.
- Check daily weight; a gain of >2lb (≈0.9kg) in 24hours signals fluid buildup.
These signs guide how aggressively you’ll need to act.
Lifestyle Measures That Make a Difference
Small daily habits can curb the fluid tide.
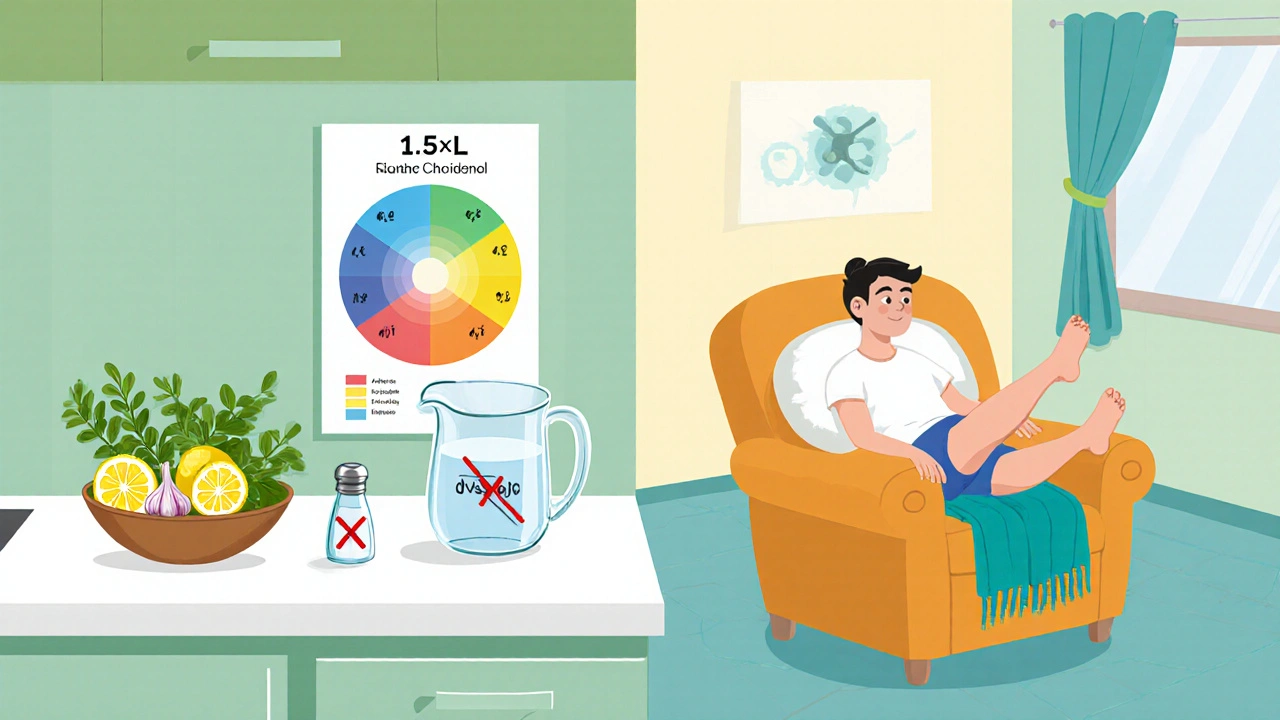
- Salt restriction: Aim for sodium restriction of ≤2g per day (about 5g of table salt). Fresh herbs, citrus, and garlic add flavor without the sodium hit.
- Fluid limits: Many clinicians recommend 1.5-2L of total fluids daily, but follow your doctor’s specific target.
- Weight monitoring: Weigh yourself at the same time each morning, after using the bathroom, on the same scale.
- Physical activity: Light walking or cardiac rehabilitation programs improve circulation and heart efficiency without over‑exertion.
- Elevate legs: Raising legs above heart level for 15‑20minutes reduces peripheral pooling.
Medication Strategies
When lifestyle tweaks aren’t enough, medicines step in.
Here’s a quick rundown of the usual drug classes and how they tackle fluid overload.
| Aspect | Loop Diuretics | Thiazide Diuretics |
|---|---|---|
| Typical agents | Furosemide, Bumetanide, Torsemide | Hydrochlorothiazide, Metolazone |
| Onset | 15‑60min (oral), <5min (IV) | 30‑120min (oral) |
| Potency | Strong - works even when kidney function is reduced | Moderate - best when kidney function is relatively preserved |
| Common side effects | Electrolyte loss (K⁺, Mg²⁺), dehydration, ototoxicity at high doses | Hyperuricemia, mild electrolyte shifts |
| Use case in CHF | First‑line for most patients with fluid overload | Adjunct when additional diuresis needed |
Beyond diuretics, two other drug families protect the heart and indirectly help fluid balance.
- ACE Inhibitors (e.g., enalapril) lower blood pressure and reduce the heart’s workload, which can lessen fluid accumulation.
- Beta Blockers (e.g., bisoprolol) improve heart pumping efficiency over time, helping the kidneys receive better perfusion.
Always discuss dose adjustments with a healthcare professional - especially if you notice dizziness, sudden weight loss, or muscle cramps.
Monitoring and Follow‑up
Consistency beats intensity. Here’s a weekly checklist you can print and stick on the fridge.
- Morning weight - note any rise >2lb.
- Blood pressure and heart rate - aim for target set by your doctor.
- Inspect for new or worsening edema.
- Record daily fluid intake (cups, soups, beverages).
- Laboratory tests (once a month): serum electrolytes, creatinine, BUN, and BNP if ordered.
If any red flag appears - rapid weight gain, persistent coughing, or swelling that doesn’t improve after a diuretic dose - call your clinic promptly.

Common Pitfalls and How to Avoid Them
- Diuretic resistance: The kidneys may adapt, making the same dose less effective. Adding a thiazide, switching loop agents, or using a higher‑dose interval can overcome resistance.
- Electrolyte imbalance: Low potassium can cause arrhythmias. Consider a potassium‑sparing agent (e.g., spironolactone) or a supplement, but only under medical supervision.
- Over‑restriction: Cutting fluids too aggressively can lead to dehydration, kidney injury, and low blood pressure. Stick to prescribed limits.
- Missing doses: Diuretics work best when taken consistently, usually in the morning to avoid nighttime bathroom trips.
Quick Management Checklist
- Daily weigh‑in - record and trend.
- Limit sodium to ≤2g/day; read labels.
- Stay within fluid limit (usually 1.5-2L).
- Take prescribed loop diuretic as directed; consider once‑daily morning dose.
- Report any >2lb weight gain or new edema within 24hours.
- Attend cardiac rehab or at least 30min of light activity most days.
Frequently Asked Questions
How much sodium is safe for a CHF patient?
Most guidelines suggest ≤2g of sodium per day (about 5g of table salt). Individual targets may vary, so follow your clinician’s advice.
Why do I gain weight overnight?
During sleep, fluid redistributes from the legs to the bloodstream, showing up as weight gain on the scale. Regular weighing helps catch this early.
Can I use over‑the‑counter diuretics?
Self‑medicating is risky. Prescription diuretics are tailored to your kidney function and heart condition. Talk to your doctor before any OTC product.
What is the role of ACE inhibitors in fluid management?
ACE inhibitors lower blood pressure and reduce the strain on the heart, which improves kidney perfusion and lessens the body’s tendency to hold onto water.
How often should I see my cardiologist?
Typically every 3‑6months, or sooner if you notice rapid weight changes, new swelling, or worsening symptoms.
Managing fluid retention in Congestive Heart Failure is a marathon, not a sprint. By combining sensible diet, disciplined weighing, and the right medication mix, you can keep the excess fluid in check and live with more comfort and freedom.



Comments
Waking up with swollen ankles feels like the universe is reminding you that your heart is overworked. The weight of each extra fluid ounce is a silent protest against the fragile rhythm of your ticker. Yet, within this struggle lies a chance to reclaim control through tiny, intentional rituals. Start your day with a calm breath, then step onto the scale with the same reverence you would reserve for an altar. Record that number like a secret password that only you and your doctor understand.
Limit sodium as if you were guarding a treasure chest, keeping the salty invader at bay. Sprinkle herbs, citrus, and garlic on your meals and let flavor dance without the sodium shackles. Keep a fluid diary-every cup, soup, and splash counts, and you’ll spot the hidden tides before they flood your veins.
Elevate those legs each evening, and imagine the excess water slipping downhill, away from your heart’s burden. Light walking isn’t just exercise; it’s a gentle river that pushes stagnant pools toward a healthier flow. Take your diuretic in the morning, and watch it work like a tide‑pulling moon, easing the night’s accumulation.
Remember, the heart, kidneys, and blood are a trio in a delicate play; when one stumbles, the others compensate, often at your expense. By mastering diet, medication, and vigilance you become the director of this drama, not a helpless audience member. Stay patient, stay consistent, and you’ll feel the swelling recede like a tide pulling back from the shore. 🙂😊
Wow, I love this guide!!! It really breaks down the steps, and it's super helpful, especially the part about daily weigh‑ins, which is a game‑changer!!! Also, the tip on using herbs instead of salt is genius, and the fluid limits are spot on, keep it up!!!
i think this is really helpful yeah its good to have a simple plan its easy to follow even if you dont have a med degree the tips on salt and weight are good too
They don't tell you that the real culprits are the shadowy elites pushing sodium in processed foods to keep us hooked on their health surveillance! The fluid limits are a smokescreen, a way to distract us while the pharmaceutical conglomerates line their pockets. Wake up, question the "guidelines" and demand true independence from the water‑hoarding cabal.
life is a river and our hearts are boats without oars the guide is a map but you must still sail
The shadows whisper, trust no fluid.
Good advice, keep it simple and stick to the plan.
But the guide ignores the real cost of meds and how many can't afford them, that's a big oversight.
Honestly this guide is a DRAMA!!! They think sprinkling herbs and walking a bit will solve the CRISIS of heart failure!!! The truth is hidden in the deep state agenda, they want you to rely on cheap tips while the big pharma laughs!!! Wake up!!!
Honestly this is just fluff, nothing works, it's all hype.