IgA Nephropathy is not a single event-it’s a slow, silent battle inside your kidneys. Every time you get a cold or sore throat, your immune system might be accidentally attacking your own kidney filters. This isn’t just about blood in the urine. It’s about whether your kidneys will last 10 years, 20 years, or fail entirely. And for the first time, we have real tools to change that outcome-not just manage symptoms, but stop the damage before it’s too late.
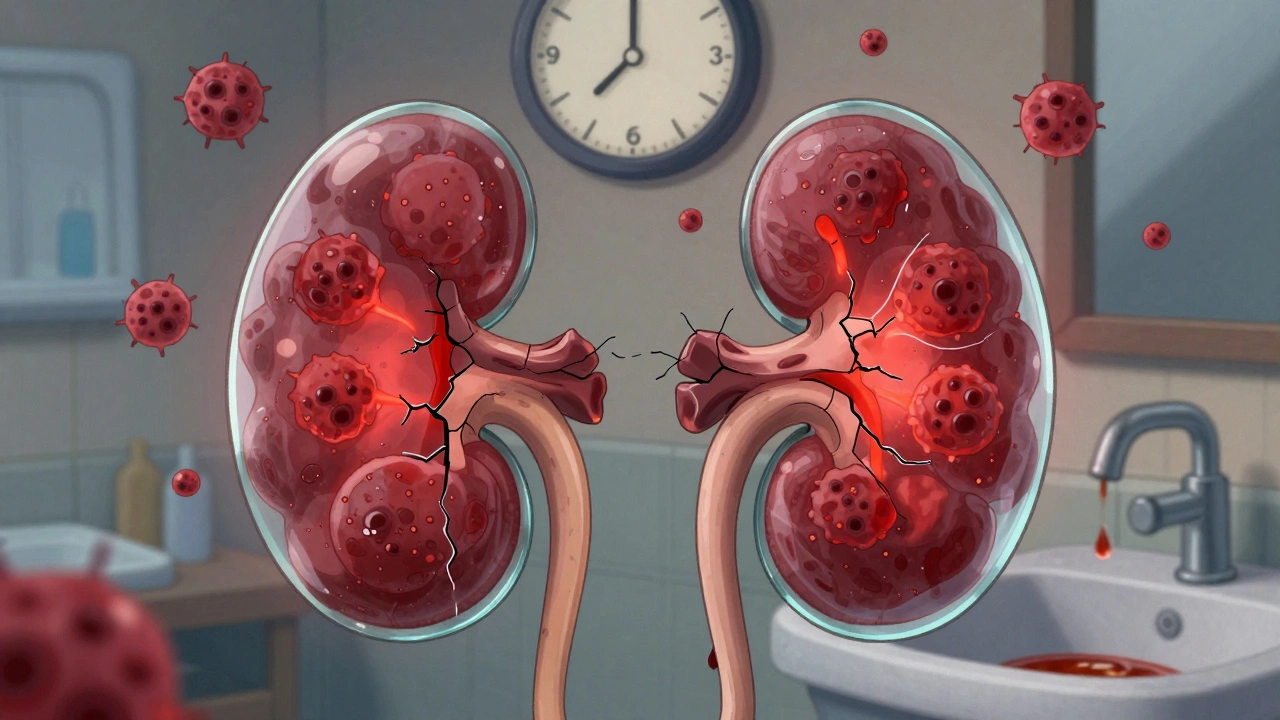
What IgA Nephropathy Actually Does to Your Kidneys
IgA Nephropathy, sometimes called Berger’s disease, starts when a faulty form of immunoglobulin A (IgA) builds up in the tiny filtering units of your kidneys-the glomeruli. These clumps trigger inflammation. Over time, scar tissue forms. Your kidneys lose their ability to clean your blood. Protein leaks into your urine. Blood appears. Your eGFR drops. And if nothing changes, you could end up needing dialysis or a transplant.
It often shows up in teens and young adults. Maybe you notice dark, cola-colored urine after a bad cold. Or maybe you don’t notice anything at all-until a routine blood test shows protein or blood in your urine. About 30-40% of cases are found this way, quietly, during check-ups. The problem? Many people wait too long to act. Until recently, doctors would watch and wait, hoping protein levels would drop on their own. Now we know: waiting lets the damage keep building.
The New Standard: KDIGO 2025 Guidelines Changed Everything
The 2025 update from Kidney Disease: Improving Global Outcomes (KDIGO) didn’t tweak the rules-it rewrote them. Before 2025, treatment was step-by-step: start with blood pressure meds (RAS inhibitors), wait 90 days, then consider steroids or other drugs if proteinuria didn’t improve. That approach ignored one critical fact: your kidneys are still being attacked during those three months.
The new guideline says: don’t wait. Start both protective and targeted therapies at the same time. That means combining:
- Medications to lower proteinuria and blood pressure (like ACE inhibitors, ARBs, or SGLT2 inhibitors)
- A drug that directly targets the IgA immune response, like Nefecon
This isn’t theory. Real-world data shows patients who got combination therapy early had significantly slower decline in kidney function. The goal? Cut proteinuria to under 0.5 grams per day. Not 1 gram. Half of what was considered acceptable just a few years ago. Why? Because even at 0.8 grams per day, 30% of patients still reached kidney failure within 10 years. That’s not stable-that’s ticking time bomb.
Nefecon: The First Drug Designed Just for IgA Nephropathy
Nefecon is the first FDA-approved drug (December 2023) that doesn’t just suppress the immune system broadly-it targets the root cause. It’s a delayed-release capsule that delivers budesonide, a steroid, directly to the gut. Why the gut? Because most of the faulty IgA in IgA Nephropathy is made there. By calming the immune cells in the intestines, Nefecon reduces the production of the harmful IgA complexes before they even reach the kidneys.
Compared to traditional oral steroids, Nefecon has far fewer side effects. In patient surveys, 72% reported less weight gain, fewer mood swings, and less trouble with blood sugar. But it’s expensive-$125,000 a year in the U.S. Many patients face insurance denials and have to appeal. That’s not a small hurdle. For many, cost is the biggest barrier to getting the best care.

Other Treatments: What Works, Where, and Why
Treatment isn’t one-size-fits-all. Geography matters. In Japan, removing the tonsils (tonsillectomy) is a common first step-studies show it reduces flare-ups and slows kidney damage in up to 60% of cases. In China, mycophenolate mofetil and hydroxychloroquine are frequently used and show strong results in clinical trials.
In Western countries, we rely more on:
- RAS inhibitors (ACE/ARBs): First-line for blood pressure and protein reduction. They’re cheap, effective, and widely available.
- SGLT2 inhibitors (like empagliflozin): Originally for diabetes, they’ve proven to protect kidneys in IgAN too-even in non-diabetics.
- Sparsentan (DEARA): Approved in Europe in 2024, this drug blocks both endothelin and angiotensin, two pathways that drive kidney scarring. It’s now an option for high-risk patients.
- Systemic steroids (prednisone): Still used, but only for patients who can’t access Nefecon or sparsentan. Long-term use brings risks: bone loss, diabetes, infections.
There’s no perfect choice. Your doctor will weigh your age, kidney function, protein levels, comorbidities, and access to drugs. A 65-year-old with diabetes might not be a good candidate for steroids. A 20-year-old athlete might prefer Nefecon over daily pills with side effects.
Prognosis: How Bad Is It Really?
Here’s the hard truth: about half of people with persistent proteinuria will lose kidney function within 10 to 20 years. But that’s not the whole story. Prognosis depends on three things:
- How much protein is leaking? Above 1 gram/day? High risk. Below 0.5? Much better outlook.
- How fast is your eGFR dropping? Losing more than 5 mL/min/year is a red flag.
- What does your kidney biopsy show? The Oxford MEST-C score grades scarring, cell growth, and other damage. More scores = higher risk.
With early, aggressive treatment, many patients stabilize. Some even see their proteinuria drop to near-normal levels. Kidney failure isn’t inevitable. But it’s still possible-especially if treatment is delayed or inconsistent.
What Patients Are Really Saying
Online communities like the IgA Nephropathy Support Group (8,500 members as of mid-2025) and Reddit’s r/kidneydisease are full of raw, honest stories. One user, GFR_Warrior, wrote: “Waiting 90 days for immunosuppression felt like watching my kidneys die slowly.” That’s why the new guideline’s simultaneous approach matters-it’s not just medical. It’s emotional.
But there’s another side. IgAN_Mom, a parent of a 16-year-old on four medications, said: “Managing the schedule is overwhelming. He’s missing school because of side effects.” Treatment burden is real. The goal isn’t just to save kidneys-it’s to preserve life. That’s why 83% of patients in a 2024 survey said quality of life matters as much as kidney function.
Access, Cost, and the Global Divide
The new treatments are revolutionary-but only if you can get them. In high-income countries, 85% of patients receive guideline-recommended care. In low- and middle-income countries? Only 22%. Nefecon costs more than most annual salaries in some regions. Tonsillectomies and mycophenolate are cheap, but they’re not widely available outside Japan and China.
Even in the U.S., only 42% of nephrology practices had fully adopted KDIGO 2025 tools by the end of 2024. Many doctors still default to old habits. Insurance companies still fight Nefecon approvals. Patients are left navigating complex appeals. This isn’t just a medical problem-it’s a systemic one.
What’s Next? The Future of IgA Nephropathy Care
Right now, 15 Phase 3 clinical trials are underway. One, called TARGET-IgAN, is testing whether biomarkers can predict who will respond to which drug-complement inhibitors, APRIL blockers, or intestinal therapies like Nefecon. Within five years, doctors might not guess your treatment. They’ll test your blood or urine and know exactly what to give you.
But progress won’t mean anything if it only helps the wealthy. The KDIGO 2025 guidelines end with a clear call: “Delay and prevent kidney failure across an entire lifetime, while minimizing treatment burden and toxicity.” That’s the goal. But achieving it means fixing access, lowering costs, and training more doctors worldwide. It’s not just science anymore. It’s justice.

Comments
It's wild how much has changed in just five years. I remember when the only advice was 'drink water and wait.' Now we have drugs that target the root cause. This isn't just progress-it's a lifeline.
Still, the cost barrier is heartbreaking. A 20-year-old shouldn't have to choose between their kidneys and their rent.
And honestly? The fact that tonsillectomies work so well in Japan but are barely discussed here says a lot about how fragmented global medicine still is.
Been following this since my diagnosis in 2021. I started on Nefecon last year. My protein dropped from 1.8 to 0.3 in six months. No weight gain. No mood swings. Just quiet, steady healing.
Insurance fought me for 11 months. Took three appeals and a letter from my nephrologist. Worth every fight.
The real paradigm shift here isn’t the drug-it’s the epistemological move from reactive to anticipatory care. We’re no longer treating biomarkers; we’re intercepting pathophysiological cascades before they crystallize into fibrosis.
That’s the future of nephrology: precision immunomodulation anchored in mucosal immunology. The gut-kidney axis isn’t metaphorical anymore-it’s therapeutic.
And yet, we’re still stuck in a fee-for-service model that penalizes early intervention. The system is designed to fail us before it’s paid to help.
My sister’s on sparsentan. She’s 28, runner, no diabetes. Used to be terrified to even get a cold. Now she’s training for a 5K.
Side effects? Mild stomach cramps for the first week. That’s it.
But she’s lucky-she’s got good insurance and a doctor who actually reads the guidelines.
Most people aren’t that lucky. And that’s the real tragedy here.
Oh wow. So now we’re giving steroids to the gut? 😏
That’s like putting duct tape on a jet engine and calling it ‘targeted therapy.’
Meanwhile, in the real world, people in India are still getting treated with nothing but ACE inhibitors and prayer. This feels less like science and more like pharma’s new luxury niche.
Also, ‘Nefecon’ sounds like a cryptocurrency. 🤡
As someone who’s spent over a decade in nephrology research, I want to emphasize: the KDIGO 2025 guidelines are the most significant update since the discovery of RAS inhibitors. This isn’t incremental-it’s foundational.
Combining SGLT2 inhibitors with Nefecon isn’t just additive-it’s synergistic. We’re seeing renal outcomes improve at a rate we haven’t seen since the 1990s with ACE inhibitors.
But you’re right, the access gap is staggering. We need global advocacy, not just clinical trials. The science is ready. The will isn’t.
I’m a nurse in Manchester. We’ve had two patients start Nefecon this year. One’s a 19-year-old uni student. The other’s a 54-year-old dad.
Both cried when they got the approval letter.
It’s not just about kidneys. It’s about being able to watch your kid graduate. Or walk your dog without feeling like you’re dying.
Thank you for writing this. People need to know this isn’t sci-fi. It’s real.
❤️
Let’s be honest: the reason so many doctors still default to the old protocol isn’t ignorance-it’s inertia. The healthcare system rewards volume over value. Monitoring proteinuria for 90 days? That’s three follow-up visits, three labs, three copays. Immediate combination therapy? One visit, one prescription, one insurance battle.
Doctors are human. They’re tired. They’re overworked. They take the path of least resistance-even when it’s the wrong one.
And patients? They’re left to navigate a labyrinth designed by bureaucrats who’ve never seen a kidney biopsy.
We need system-level change, not just guideline updates. The guidelines are the easy part. The system? That’s the real disease.
Wow. Just wow.
So now we’re supposed to believe that a $125,000 pill is the answer to a disease that’s been around since 1968?
Meanwhile, people in Nigeria are dying because they can’t afford a single dose of prednisone.
This isn’t medicine. It’s capitalism with a stethoscope.
And you call this progress? I call it exploitation dressed in peer-reviewed journals.
Stop patting yourselves on the back. Start fighting for equity.
💔
My 16-year-old son has IgAN. He’s on Nefecon, an SGLT2i, and an ARB. He’s missed 17 days of school this year because of fatigue and nausea.
He says he doesn’t care if he lives to 30 as long as he doesn’t feel like he’s dying every day.
We’re lucky we can afford this. But what about the kid whose mom works two jobs and can’t take a day off to fight insurance?
Science is amazing. But humanity? We’re still failing.
I’m so tired.
Just wanted to say thank you for writing this. I’m a 32-year-old with IgAN. Diagnosed at 26. Was told ‘you’ll be fine’ for three years. Then my eGFR dropped to 58.
I found this article after a Google spiral at 3 a.m. It was the first time I felt seen.
I started Nefecon last month. First week: tired. Second week: less swelling. Third week: I slept through the night.
It’s not magic. But it’s hope.
And hope? That’s worth fighting for.
I’ve had this since I was 18. Now I’m 41. I’ve been on every drug under the sun. Steroids made me gain 60 pounds. My bones are brittle. My mood is a rollercoaster.
I lost my job because I couldn’t show up. My wife left. My kids don’t know me.
They tell me ‘early intervention’ now. But what about the people who were told to wait? Who waited too long?
They don’t talk about the ones who didn’t make it.
They just write papers.
I’m tired of being a statistic.
My dad’s a nephrologist. He’s been treating IgAN since the 90s. He told me last night: ‘I used to tell patients they’d be fine. Now I tell them: we can stop this. But you have to move fast.’
He’s never cried in front of me before.
But he cried when he read the new guidelines.
It’s not just science. It’s redemption.