Most people know that high blood pressure can hurt your heart or kidneys. But few realize it’s quietly damaging the tiny blood vessels in your eyes-sometimes long before you notice any vision problems. Hypertensive retinopathy isn’t just a medical term; it’s a warning sign your body is under serious stress. And if left unchecked, it can lead to permanent vision loss.
What Exactly Is Hypertensive Retinopathy?
Hypertensive retinopathy happens when high blood pressure damages the blood vessels in your retina-the light-sensitive layer at the back of your eye. These vessels are delicate. When pressure pushes through them too hard for too long, their walls thicken, narrow, and eventually leak. Blood and fluid spill into the retina, blocking vision. It’s not sudden. It builds over years.
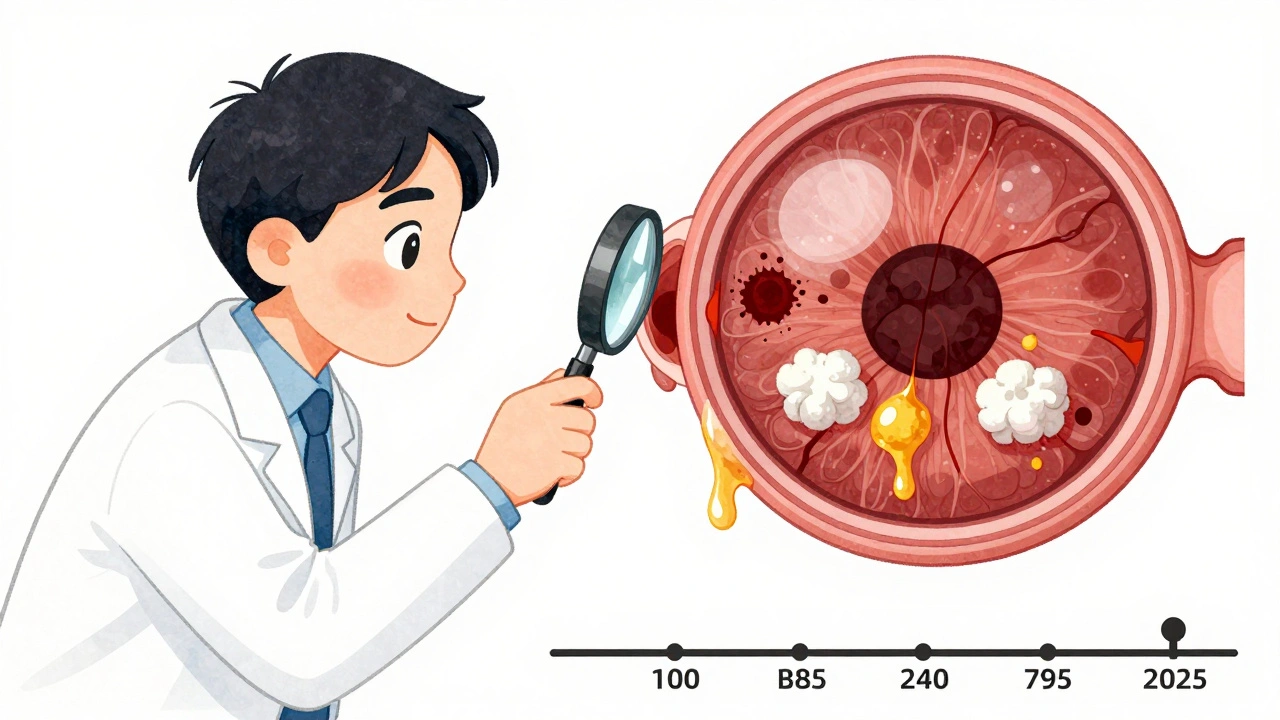
The damage shows up in predictable patterns. Doctors use the Keith-Wagener-Barker (KWB) system to grade it in four stages. Stage 1? Just slight narrowing of the arteries. You won’t feel anything. Stage 2? Arteries start crossing veins, pinching them-called arteriovenous nicking. Still no symptoms. By Stage 3, you see hemorrhages, cotton wool spots (tiny white patches from nerve damage), and hard exudates (yellow lipid deposits). That’s when vision blurs. Stage 4? Swelling of the optic nerve (papilledema). This is an emergency. It means your blood pressure is dangerously high, and your brain might be at risk too.
How High Does Blood Pressure Have to Be to Cause Damage?
There’s no magic number, but the risk climbs sharply when systolic pressure hits 140 mmHg or higher. The CDC says nearly 1 in 3 U.S. adults have stage 2 hypertension-that’s 140/90 or above. And about 13.9% of them already have retinal changes.
Even “mild” hypertension-130-139 systolic-can cause damage if it lasts more than 10 years. A 2023 study from the Merck Manual found that retinal changes appear in 22% of patients after just three years of uncontrolled high blood pressure. That’s faster than most people expect.
When systolic pressure spikes above 180 mmHg, retinal hemorrhages show up in 35% of patients. Diastolic pressure over 120 mmHg can trigger optic nerve swelling in 40% of cases within just 48 hours. These aren’t rare events. They’re predictable outcomes of untreated hypertension.
Why You Might Not Notice It Until It’s Too Late
Here’s the scary part: 68% of people with early-stage retinopathy (Grades 1-2) feel nothing. No pain. No blurriness. No flashes. Your eyes don’t hurt. That’s why so many wait until vision is already fading before they get checked.
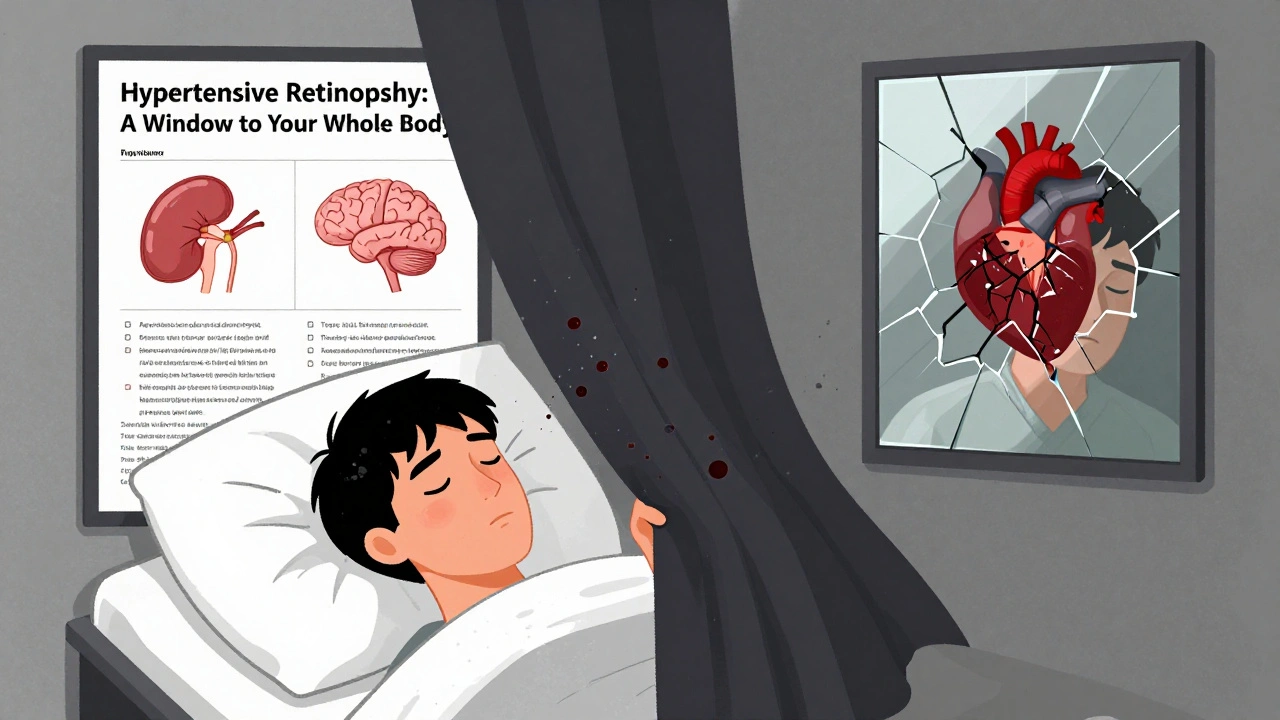
By the time symptoms appear-blurred vision, dark spots, sudden vision loss-it’s often Grade 3 or 4. Patients describe it as a “curtain” falling over their vision. One Reddit user wrote: “Woke up with dark spots after my BP hit 210/110.” Another said, “Double vision and a headache so bad I thought I was having a stroke.”
And they’re right to worry. Grade 4 retinopathy isn’t just an eye problem. It’s a red flag for stroke, heart attack, and kidney failure. People with papilledema have a 78% higher risk of stroke. The retina is a window into your whole vascular system. If it’s damaged, so are your arteries elsewhere.
How Doctors Spot It-Before You Can
There’s no blood test for hypertensive retinopathy. The only way to see it is with an eye exam. A simple fundoscopic exam, where the doctor shines a light into your eye and looks at the retina, can catch changes at Stage 1.
Now, many clinics use optical coherence tomography (OCT)-a non-invasive scan that shows retinal thickness and fluid buildup. OCT can detect swelling as small as 10-15% increase in thickness. AI tools like RetinaCheck AI, cleared by the FDA in 2022, now help analyze images with 92% accuracy-up from 75% just a few years ago.
Doctors don’t wait for symptoms. If you have stage 2 hypertension, they should be checking your eyes at least once a year. For resistant hypertension-blood pressure still high despite three medications-the American Heart Association now recommends scans every six months.
Can You Reverse the Damage?
Yes-but only if you act fast. The key is lowering blood pressure, and doing it safely. Rushing to drop pressure too fast can cause more damage. The goal is a controlled reduction: lowering systolic by about 25 mmHg in the first 24-48 hours.
Studies show that when this is done properly, 65% of acute retinal changes improve within days. Hemorrhages clear. Exudates shrink. Vision starts to come back in 7-10 days. But if the macula (the center of your vision) is damaged, recovery can take 3-6 months-and even then, 22% of patients are left with permanent blind spots.
Medications matter too. A 2023 European Society of Cardiology study found ACE inhibitors reduce retinal damage progression by 32% compared to calcium channel blockers. That’s a big difference. If you’re on blood pressure meds, ask your doctor if yours are the best for your eyes.
What You Can Do Right Now
1. Know your numbers. Check your blood pressure at home. Use a validated device. Record readings for a week. Don’t guess.
2. Get your eyes checked. If you have high blood pressure, schedule a dilated eye exam-even if you see fine. No excuses.
3. Take your meds. Adherence drops to 30% in many patients. But those who take their pills and get regular eye exams have 35% better BP control.
4. Watch for warning signs. Blurry vision, floaters, sudden blind spots, double vision, or severe headaches? Don’t wait. Call your doctor or go to urgent care.
5. Don’t ignore “mild” hypertension. Even 130-139 systolic over 10 years can hurt your eyes. Early action prevents late consequences.
The Bigger Picture: It’s Not Just About Your Eyes
Hypertensive retinopathy is more than an eye disease. It’s a sign your entire vascular system is under siege. People with retinal damage have 2.5 times the risk of heart attack or stroke. That’s why doctors call it a “window to systemic health.”
And if you have diabetes too? Your risk of permanent vision loss jumps 4.7 times. Combined retinopathies are brutal. Managing both conditions isn’t optional-it’s survival.
Research is moving fast. The NIH is now studying genetic markers that predict who’s most vulnerable. New devices like RetiFlow can measure retinal blood flow without dye injections. In five years, we may be able to predict who’s at risk before any damage even starts.
But for now, the tools we have are simple: know your pressure, get your eyes checked, take your meds, and don’t wait for symptoms. Your vision isn’t just about reading or driving. It’s about living without fear. And that starts with a single step-seeing your doctor before it’s too late.



Comments
This is the kind of post that makes you pause and check your blood pressure right now
Didn't realize my eyes could be screaming for help while I felt fine
soooooo i heard from my cousin’s neighbor’s dog walker that eye damage from high bp is actually caused by too much coffee?? like 3 lattes a day?? and that’s why the doc says ‘check your eyes’?? idk but i think this whole thing is a big pharma scam to sell more meds lol
While the post is accurate, it’s worth noting that retinal changes can appear even in prehypertension - especially in those with diabetes, chronic kidney disease, or autoimmune conditions. The 2023 Merck Manual data cited is solid, but population-level studies often miss subgroups. For example, Black and South Asian patients show earlier retinal microvascular changes at lower BP thresholds. Regular fundoscopy isn’t just recommended - it’s essential for anyone with sustained systolic pressure above 130. And yes, ACE inhibitors do have a measurable advantage in retinal protection - not just for BP control, but for endothelial repair. Don’t assume ‘no symptoms’ means ‘no damage.’
Ugh. Another ‘check your BP’ lecture. Like we don’t already know. My grandma died of a stroke because she ignored this. And now we’re supposed to feel guilty? Thanks for the guilt trip, doc. I’ll just keep ignoring it like everyone else. At least I’m not paying $800 for an ‘OCT scan’ when my insurance won’t cover it. #FirstWorldProblems
Thank you for writing this with such clarity - it’s rare to see medical info that doesn’t make you feel like you’re failing just for existing
Small steps matter - even checking your pressure once a week is a win
And if you’ve got meds, take them like you’re brushing your teeth - not because you have to, but because you care about your future self
You’re not broken. You’re just human. And humans need help sometimes. That’s okay
Exactly. I’ve seen too many patients wait until they’re losing vision to come in. And then we scramble. The retina is the only place in the body where you can see live blood vessels without surgery. If they’re narrowing, leaking, or bursting - your heart, kidneys, and brain are already under siege. Don’t wait for the curtain to fall. Get the exam. Track your numbers. Take the pill. It’s not about fear. It’s about agency. You still have control. Use it.
Oh wow, another American medical horror story. In India, we don’t need fancy OCT scans - our grandmothers knew hypertension was a silent killer by watching the eyes. No technology needed. Just common sense. You people treat medicine like a subscription service. Fix your diet. Walk. Stop stress-eating. And stop paying for tests you don’t need.
It’s wild how the eye becomes this silent witness to systemic decay - like your body’s own documentary camera recording every spike, every ignored warning, every missed appointment
What’s even more haunting is that the retina doesn’t lie. It doesn’t care if you’re busy, stressed, or broke. It just shows you what’s happening - if you’re willing to look
If we could see our arteries like we see our retinas - if every person could look into a mirror and see the slow collapse of their own vessels - would we still treat our bodies like disposable machines?
Maybe this isn’t about medicine at all.
Maybe it’s about how we’ve lost the habit of listening - to our bodies, to our ancestors, to the quiet signals before the scream.
bro i just checked my bp and it was 138/89
so like… do i need to go to the eye doctor or nah?? i mean i can still see my phone just fine
also why is everyone so serious about this??