Digoxin-Amiodarone Dose Adjustment Calculator
Critical Safety Guide
- 35% increased 30-day mortality in heart failure patients
- 2.1x higher stroke risk
- Life-threatening arrhythmias and toxicity
Digoxin Dose Adjustment Calculator
Enter your patient's current digoxin dose in micrograms per day (mcg/day).
Recommended Digoxin Dose
Important: Recheck digoxin levels at 72 hours and adjust as needed. Amiodarone's metabolite remains active for up to 100 days.
Key Clinical Data: When clinicians reduce digoxin dose by 50% after starting amiodarone, toxicity rates drop from 12.3% to 2.1% (UCSF study).
Why This Drug Combo Can Be Deadly
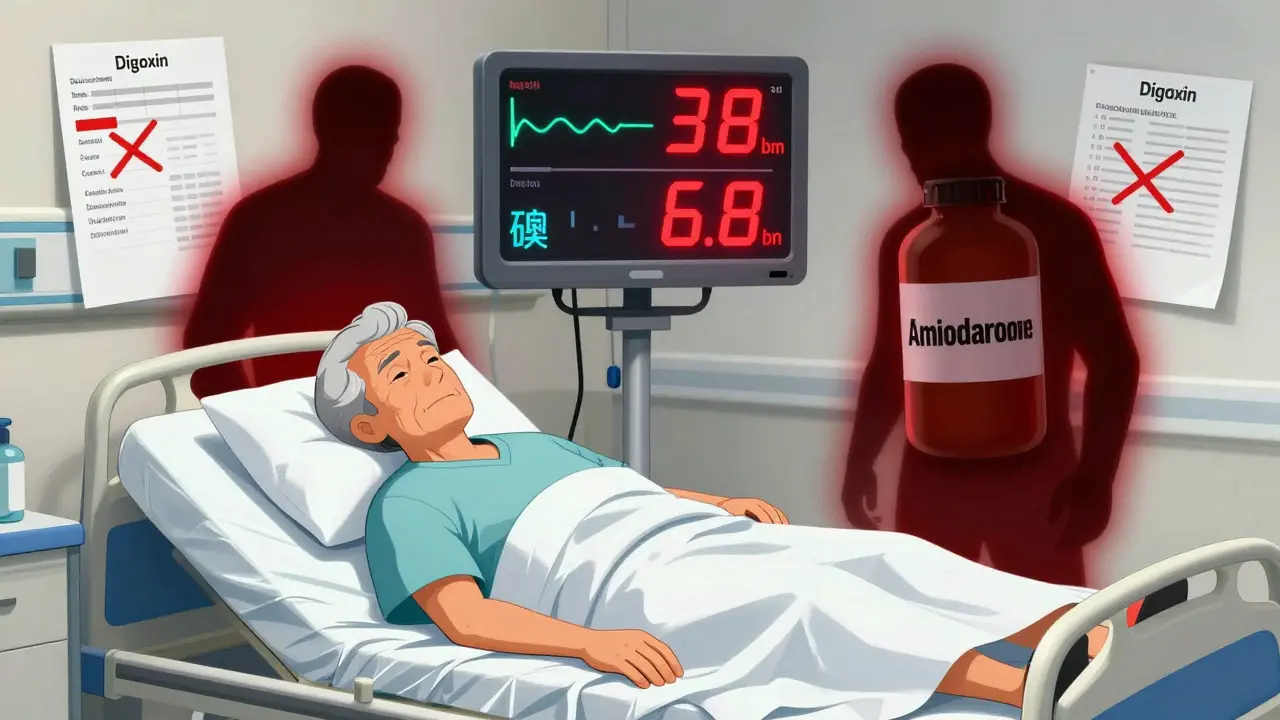
Imagine you’re treating a 78-year-old patient with atrial fibrillation and heart failure. You start amiodarone to control the rhythm. Everything seems fine-until three days later, they collapse. Their heart rate drops to 38 beats per minute. Their potassium soars to 6.8. They’re in the ICU. The cause? A simple oversight: no one reduced the digoxin dose.
This isn’t a rare mistake. It happens more often than you think. Digoxin and amiodarone are both lifesaving drugs-but together, they’re a ticking time bomb. Both have narrow therapeutic indices, meaning the difference between a helpful dose and a toxic one is razor-thin. Digoxin’s safe range? Just 0.5 to 0.9 ng/mL. Go above that, and you risk fatal arrhythmias, nausea, vision changes, or even death. Amiodarone doesn’t just add to the risk-it multiplies it.
How Amiodarone Turns Digoxin Into a Poison
Amiodarone doesn’t just sit there. It actively changes how digoxin behaves in the body. The main culprit? P-glycoprotein. This protein acts like a bouncer at the cell door, kicking digoxin out of tissues and into the bloodstream for removal. Amiodarone shuts down this bouncer. As a result, digoxin piles up-sometimes doubling in concentration.
Studies show that when amiodarone is added, digoxin levels jump from an average of 0.97 ng/mL to nearly 2.0 ng/mL. That’s more than double the upper limit of safety. Even worse, this doesn’t happen overnight. The peak effect takes 1 to 2 weeks. Many doctors check a digoxin level before starting amiodarone, then assume they’re safe because the initial number looks fine. They’re wrong. The real danger is hidden, waiting to explode.
Amiodarone’s long half-life-up to 100 days-means this risk doesn’t vanish when you stop the drug. Desethylamiodarone, its active metabolite, keeps blocking P-glycoprotein for weeks or even months. So if a patient was on amiodarone six weeks ago and now needs digoxin? Still risky.
The Numbers Don’t Lie: How Often This Kills
Back in 1984, a landmark study showed that 32% of patients on both drugs developed gastrointestinal toxicity. Nearly 18% had neurological symptoms. That’s nearly one in three. Fast forward to 2021, and a large cohort study found this combo led to 2.3 times more hospitalizations than other common drug pairs like digoxin and furosemide.
But the scariest data? A 2021 JACC: Heart Failure analysis showed that when doctors didn’t reduce digoxin after starting amiodarone, 35% of heart failure patients died within 30 days. That’s up from 8% when the dose was adjusted. That’s a 27-point absolute increase in death risk. No other common cardiac interaction carries that kind of mortality penalty.
And it’s not just hospital stays or death. A 2024 Circulation study linked the combo to a 2.1-fold higher stroke risk. Why? Elevated digoxin may trigger prothrombotic effects-making blood clots more likely. This isn’t just about arrhythmias anymore. It’s about strokes, kidney failure, and sudden cardiac arrest.

What Doctors Are Doing Right (and Wrong)
Here’s the brutal truth: most clinicians still get this wrong. A 2022 study across 15 U.S. hospitals found only 44% of patients had their digoxin dose cut when amiodarone was started. In community hospitals? The error rate hit 68%.
Why? Because it’s easy to forget. Amiodarone is often added in an emergency. Digoxin has been on the chart for months. The assumption is, “It’s been fine so far.” But that’s exactly when it’s most dangerous.
Some institutions are fixing this. At UCSF, they now require:
- Check digoxin level before starting amiodarone
- Immediately reduce digoxin by 50%
- Recheck levels at 72 hours
At the VA, they added an EHR alert. If both drugs are ordered together, the system pops up: “Dose reduction required. Digoxin must be cut by 50%.” Result? A 41% drop in toxicity events.
But in most places? No alert. No protocol. Just hope.
Exactly How to Adjust the Dose
There’s no guesswork here. The guidelines are clear:
- Before starting amiodarone: Measure the current digoxin level. Don’t skip this-even if it’s been stable for years.
- At initiation: Reduce digoxin by 50%. That’s it. Don’t wait for the next level. Don’t wait for symptoms. Start the reduction immediately.
- For patients with kidney problems (CrCl <50 mL/min): Cut it to 33% of the original dose. Their bodies clear digoxin slower anyway. Add extra risk? Don’t take the chance.
- Recheck levels: At 72 hours. If still above 0.9 ng/mL, reduce further. If below 0.5 ng/mL, you might need to increase slightly-but only if the arrhythmia is still uncontrolled.
- After stopping amiodarone: Wait at least 60 days before considering a digoxin dose increase. The metabolite lingers.
Don’t rely on symptoms. Nausea, blurred yellow vision, or a slow pulse? Those are late signs. By then, damage is done.
Who’s at Highest Risk?
This isn’t a one-size-fits-all interaction. Some patients are walking into a minefield:
- Patients over 75-their kidneys don’t clear digoxin well.
- Those with CKD stage 3 or worse-every 10-point drop in eGFR increases digoxin toxicity risk by 20%.
- People on diuretics-low potassium or magnesium makes digoxin toxicity more likely to trigger deadly rhythms.
- Those with recent heart failure hospitalizations-they’re already fragile. Adding this combo is like pouring gasoline on a fire.
One cardiologist on Reddit said he’s seen three digoxin toxicity cases in the past year-all in patients over 75 with chronic kidney disease. That’s not coincidence. That’s pattern.
What to Do Instead
Maybe you don’t need digoxin at all. The 2024 European Society of Cardiology guidelines now recommend beta-blockers or calcium channel blockers (like diltiazem or verapamil) as first-line for rate control in atrial fibrillation-even if you’re planning to use amiodarone.
Why stick with digoxin if safer options exist? Digoxin doesn’t improve survival. It just helps with symptoms. If you’re using it for rate control, there are better, safer alternatives.
But if you’re using digoxin for heart failure with reduced ejection fraction? Then it’s still valuable. Just manage the interaction like your patient’s life depends on it-because it does.
The Bottom Line
This interaction isn’t theoretical. It’s killing people right now. Every time a doctor starts amiodarone without reducing digoxin, they’re gambling with a patient’s life. The science is settled. The guidelines are clear. The tools are available.
So here’s what you do:
- If you’re prescribing amiodarone to someone on digoxin-reduce the digoxin dose by 50% on day one.
- If you’re prescribing digoxin to someone who’s taken amiodarone in the last two months-assume toxicity risk until proven otherwise.
- If you’re not using an EHR alert-push for one.
- If you’re not checking levels after the change-start.
There’s no excuse for missing this. It’s not complex. It’s not controversial. It’s just ignored. And people are dying because of it.
Why is the digoxin-amiodarone interaction so dangerous compared to other drug combos?
This combo is uniquely dangerous because both drugs have narrow therapeutic windows, and amiodarone doesn’t just mildly increase digoxin levels-it can double them. Unlike interactions with antibiotics or diuretics, this one affects multiple clearance pathways (P-glycoprotein and CYP3A4), making it harder to predict and reverse. The risk of fatal arrhythmias, kidney failure, and death is significantly higher than with other common cardiac drug pairs.
How soon after starting amiodarone should digoxin levels be checked?
Check the digoxin level immediately before starting amiodarone, then again at 72 hours after initiation. The peak increase in digoxin concentration typically occurs between 1 and 2 weeks, but toxicity can appear as early as 48 hours. Waiting longer than 72 hours risks missing the window to prevent harm.
Should I stop digoxin completely when starting amiodarone?
No. Stopping digoxin entirely is usually unnecessary and can worsen heart failure or atrial fibrillation control. Instead, reduce the dose by 50% (or 33% if kidney function is impaired). This balances safety with therapeutic benefit. Recheck levels and adjust further only if needed.
Can I use dronedarone instead of amiodarone to avoid this interaction?
No. Dronedarone, a cousin of amiodarone, carries similar risks. The PALLAS trial showed dronedarone increased cardiovascular death when combined with digoxin. The mechanism is nearly identical-P-glycoprotein inhibition. So switching to dronedarone doesn’t solve the problem. Avoid digoxin entirely if possible.
What if a patient has been on amiodarone for months and now needs digoxin?
Treat it as if they’re still on amiodarone. The active metabolite, desethylamiodarone, can linger for up to 60 days after stopping. Always assume the interaction is active unless it’s been over two months since the last dose. Start with a 50% digoxin reduction and monitor levels closely.
Are there alternatives to digoxin for heart failure patients on amiodarone?
For rate control in atrial fibrillation, beta-blockers (like metoprolol) or non-dihydropyridine calcium channel blockers (like diltiazem) are safer and equally effective. For heart failure with reduced ejection fraction, SGLT2 inhibitors (like dapagliflozin) and ARNIs (like sacubitril/valsartan) now have stronger evidence for survival benefit than digoxin. Consider these before reaching for digoxin.
What Comes Next?
Research is still evolving. The DIG-AMIO trial (NCT05217891), which started in 2023, is comparing 50% versus 33% digoxin dose reductions with amiodarone initiation. Results are expected in late 2025. Meanwhile, newer drugs like vericiguat and omecamtiv mecarbil are showing promise in heart failure without the toxicity risks of digoxin.
But for now, the solution is simple: reduce the dose. Check the level. Don’t wait. Don’t assume. The data is clear. The lives saved depend on it.

Comments
I can't believe this still happens... I work in med-surg and saw a patient go into torsades because no one reduced digoxin after amiodarone. It was terrifying. Why aren't we automating this??
P-gp inhibition + narrow TI = perfect storm. Amiodarone's metabolite has a longer half-life than the patient's memory of their med list. This isn't just a drug interaction-it's a systems failure.
So... we're saying if you're on amiodarone, digoxin is basically a loaded gun? And we're still not putting up alerts? Bro. We have self-driving cars. We can't auto-flag this?
I've seen this twice in my rotation. One patient survived because the pharmacist caught it. The other didn't. The difference? One had a clinical pharmacist on the team. The other didn't. It's not about knowledge-it's about structure.
In India we don't even have digoxin levels checked routinely. Amiodarone is given like aspirin. If the patient dies, it's 'natural causes'. This is why Western medicine is overcomplicating things.
Digoxin and amiodarone... like two old lovers who used to dance together perfectly-until one started drinking and forgot how to step... now the whole house is on fire and no one knows who brought the matches
This is a textbook example of why clinical protocols must be standardized. The 50% reduction rule isn't optional-it's evidence-based, life-saving, and shockingly underutilized.
Let me guess-next they'll tell us oxygen is dangerous for COPD patients. This is just fear-mongering dressed up as medicine. People have been on this combo for decades. Where's the data that says we're killing them by accident?
You know what's worse than this interaction? The fact that doctors still think they can remember every single drug interaction in their head. We have computers now. We have AI. We have apps that can warn us. But no, we still rely on the human brain that forgets where it put its keys five minutes ago.
To the person who said 'it's been fine for years'-that’s the exact phrase that kills people. You don’t get a second chance when digoxin toxicity hits. This isn’t a suggestion. It’s a mandate.
I had a patient last month. Got amiodarone, digoxin stayed at 0.125mg. Level went from 0.8 to 2.1 in 10 days. We caught it because the nurse noticed he was seeing halos. That’s the kind of thing you don’t unsee.
I'm just glad we're talking about this. Too many of these stories die in chart notes. If this saves one life, it's worth the post. Thank you for writing this.