Managing bipolar disorder isn’t about finding one magic pill. It’s about balancing effectiveness with tolerability-because the drugs that help control wild mood swings often come with side effects that can make life harder, not easier. For many people, the goal isn’t just to stop manic episodes or lift depression. It’s to live a life where you don’t feel like you’re constantly fighting your own brain.
What Are Mood Stabilizers, Really?
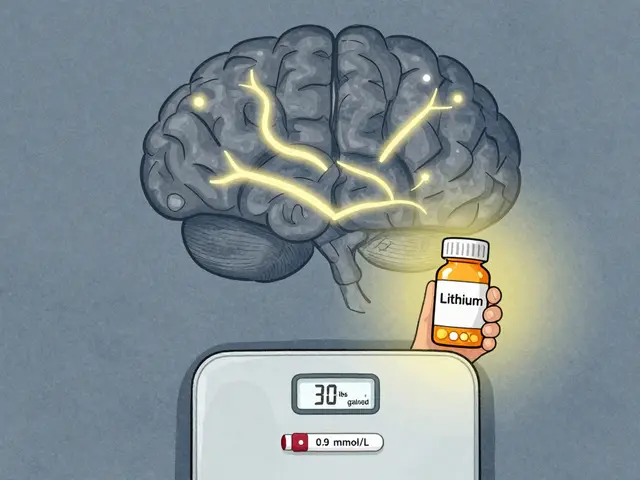
Mood stabilizers are the backbone of long-term bipolar treatment. They don’t just calm highs or lift lows-they help prevent both from happening in the first place. Lithium, approved by the FDA in 1970, is still the most studied and trusted option. It doesn’t work like an antidepressant or a sedative. Instead, it seems to stabilize the brain’s electrical activity over time, reducing the frequency and intensity of episodes.
But lithium isn’t simple. You need regular blood tests to make sure you’re in the sweet spot: 0.6 to 1.0 mmol/L for maintenance, and 0.8 to 1.0 mmol/L during acute mania. Go above 1.2 mmol/L, and you risk toxicity-symptoms like slurred speech, shaky hands, or even seizures. Most people start at 300 mg a day and slowly increase every few days, based on blood levels and how they feel. Side effects? Nearly everyone deals with something: frequent urination (30-40% of users), hand tremors (up to half), weight gain (10-15 pounds in the first year), and nausea.
Other mood stabilizers include valproate, carbamazepine, and lamotrigine. Valproate works fast for mania but carries serious risks for women of childbearing age-it can cause birth defects. Lamotrigine is the go-to for depression in bipolar disorder, with a 47% response rate compared to 28% for placebo. But it comes with a warning: a rare but dangerous skin rash affects about 1 in 10 people. That’s why doctors start low and go slow-sometimes taking weeks just to reach a safe dose.
Antipsychotics: Fast Relief, Heavy Costs
Atypical antipsychotics like quetiapine, olanzapine, and aripiprazole were originally designed for schizophrenia. But they turned out to be powerful tools for bipolar disorder too. Quetiapine (Seroquel) got FDA approval for bipolar depression in 2006, and it’s now one of the most prescribed meds for the condition. Why? Because it works fast. People often feel better within 7 days, while lithium can take two weeks or more.
But speed comes with a price. Quetiapine causes drowsiness in 60-70% of users. Weight gain is common-on average, 22 pounds over a year, according to patient reports. Olanzapine is even worse for metabolism: it increases the risk of type 2 diabetes by 20-30%. Aripiprazole (Abilify) and lurasidone (Latuda) are better choices if you’re worried about weight or blood sugar-they cause minimal weight gain. In 2023, the FDA approved lumateperone (Caplyta) for bipolar depression with just 0.8 kg of weight gain at six weeks, compared to 3.5 kg with quetiapine.
Antipsychotics also help with acute mania. Risperidone shows a 68% response rate in just three weeks. But long-term use? Many people quit because of side effects: sedation, restlessness (akathisia), or feeling emotionally flat. One Reddit user wrote: “I stopped quetiapine because I felt like a zombie. I wasn’t manic, but I wasn’t me either.”
Combining Medications: When Two Are Better Than One
Many people don’t respond to a single drug. That’s where combination therapy comes in. Adding an antipsychotic to a mood stabilizer boosts response rates to 70% in treatment-resistant cases. But it also bumps up side effects by 25-30%. A patient on lithium and quetiapine might get stable moods-but also gain 30 pounds, feel constantly tired, and struggle with blood sugar spikes.
Doctors try to avoid stacking meds unless necessary. But for those with frequent hospitalizations, suicidal thoughts, or rapid cycling, the benefits often outweigh the risks. The key is monitoring. Quarterly blood tests for glucose, cholesterol, and liver function. Tracking waist size and BMI. Catching metabolic issues early can prevent diabetes or heart disease down the road.
Why Do So Many People Stop Taking Their Meds?
Studies show 40% of people with bipolar disorder stop their medication within a year. The National Alliance on Mental Illness found that 45% of 1,200 surveyed patients quit because of side effects. The top reasons? Weight gain (78%), brain fog (65%), and sexual dysfunction (52%).
One person on PatientsLikeMe said: “I was happier on lithium than I’d been in years-but I couldn’t look in the mirror anymore.” Another wrote: “I took lamotrigine for two months. No mania, no depression. But I couldn’t sleep. Not a single night. I quit.”
But not everyone has a bad experience. A different Reddit user with 85 upvotes shared: “After three meds failed, lithium finally worked. I gained 15 pounds. But I haven’t had a suicidal episode in two years. That’s worth it.”
It’s not about being weak or non-compliant. It’s about quality of life. If the medicine makes you feel worse than your illness, you’ll find a way to stop it-no matter how much your doctor insists.
What About Antidepressants?
This is one of the most debated topics in bipolar care. Antidepressants like fluoxetine (Prozac) can lift depression-but they can also trigger mania. Studies show a 10-15% risk of switching into mania, and up to 25% if used alone. That’s why experts almost always recommend pairing them with a mood stabilizer.
Some psychiatrists avoid them entirely. Dr. Gary Sachs from Harvard warns that antidepressants can worsen cycling over time. Others, like Dr. David Miklowitz at UCLA, say they’re safe if used carefully and short-term for severe depression.
The bottom line? Don’t take an antidepressant unless you’re already on a mood stabilizer-and even then, monitor closely. If you feel unusually energetic, impulsive, or irritable after starting an antidepressant, call your doctor. That’s not improvement-that’s a red flag.

Practical Tips for Staying on Track
Medication management isn’t just about prescriptions. It’s about daily habits and communication.
- Take lithium with food. Reduces nausea and helps absorption.
- Split doses. Taking lithium twice a day (instead of once) can reduce side effects like tremors.
- Use metformin. Many doctors prescribe this diabetes drug to counteract weight gain from antipsychotics.
- Track your mood. Use a simple app or journal. Note sleep, energy, irritability. Patterns matter more than single days.
- Don’t mix NSAIDs. Ibuprofen, naproxen, and even aspirin can spike lithium levels to dangerous ranges. Use acetaminophen instead for pain.
- Get blood tests. Weekly at first. Every 2-3 months once stable. Never skip them.
And don’t be afraid to speak up. If your doctor says, “This is the only option,” ask: “Is there another with fewer side effects?” There almost always is.
The Future: Personalized Treatment Is Here
Genetic testing is starting to change the game. Companies like Genomind test for variations in CYP2D6 and CYP2C19 genes-enzymes that break down 40% of bipolar medications. If your body processes lithium slowly, you might need half the dose. If you’re a fast metabolizer of quetiapine, you might need more. These tests aren’t perfect-but they improve medication selection by 30%, according to a 2021 study.
Long-acting injectables are also growing. Abilify Maintena, given once a month, helps people who struggle with daily pills. And new drugs like cariprazine and lurasidone are gaining favor for bipolar depression because they don’t wreck your metabolism.
Even digital tools are helping. reSET-BD, a smartphone app approved by the FDA, helps patients track symptoms and stick to treatment. In trials, it cut relapse rates by 22%.
But here’s the truth: no matter how advanced the science gets, lithium remains the most effective drug for preventing suicide in bipolar disorder. Studies show it reduces suicide risk by 80% compared to placebo. That’s why experts still call it the gold standard-even with its side effects.
What Success Looks Like
Success isn’t about being perfectly calm all the time. It’s about fewer hospital visits. Fewer days lost to depression. More time with family. More ability to hold a job. More days where you wake up and don’t dread what’s coming.
Only 35% of people with bipolar disorder reach full remission. Six in ten still struggle with side effects that need medical attention. But those who stick with a tailored plan-monitoring closely, adjusting when needed, and speaking up about how they feel-are the ones who thrive.
There’s no perfect drug. But there is a right path-for you. It takes patience, honesty, and a team that listens. And it’s worth it.
Can I take mood stabilizers and antipsychotics together?
Yes, many people take both, especially if one drug alone isn’t enough. Combining a mood stabilizer like lithium with an antipsychotic like quetiapine can improve symptom control by up to 70%. But it also increases side effects-like weight gain, drowsiness, and metabolic issues-by 25-30%. Your doctor will monitor you closely for these, and may adjust doses to balance effectiveness and tolerability.
Which is better for bipolar depression: lithium or quetiapine?
Quetiapine works faster-many people feel better within a week. Lithium takes longer, often 2-4 weeks. But lithium is more effective at preventing future episodes and reducing suicide risk. Quetiapine is better for acute depression, while lithium is better for long-term stability. Some people take both: quetiapine to get out of a depressive episode, then switch to lithium for maintenance.
Why do I need blood tests if I feel fine?
Mood stabilizers like lithium have a narrow safety window. You can feel fine but still be in the danger zone-levels above 1.2 mmol/L can cause toxicity without obvious symptoms at first. Blood tests catch this early. Even if you feel good, skipping tests puts you at risk for kidney damage, thyroid problems, or sudden neurological issues. Weekly tests at first, then every 2-3 months, are standard and life-saving.
Can I stop my meds if I feel better?
No-not without talking to your doctor. Stopping suddenly can trigger a rebound episode, sometimes worse than before. Bipolar disorder is a chronic condition. Medication doesn’t cure it; it manages it. Even if you’ve been stable for a year, stopping increases your relapse risk by 50-70%. If side effects are unbearable, work with your provider to switch or adjust-not quit.
Are there natural alternatives to these medications?
There’s no proven natural substitute for mood stabilizers or antipsychotics in bipolar disorder. Omega-3s, magnesium, and mindfulness can help with general mood support, but they don’t prevent mania or severe depression. Relying on them instead of medication has led to hospitalizations and suicide attempts. Use supplements only as add-ons-not replacements. Always tell your doctor what you’re taking, even if it’s “natural.”
How do I know if my medication isn’t working?
If you’re having frequent mood episodes-like two or more manic or depressive episodes in a year-or if you’re still struggling with daily functioning despite taking your meds, it’s likely not working well enough. Also, if side effects are so bad you’re skipping doses or thinking about quitting, that’s a sign it’s time to talk to your doctor. Don’t wait until you’re in crisis. Early adjustments lead to better outcomes.


Comments
I’ve been on lithium for 5 years. Tremors? Yeah. Weight gain? 20 lbs. But I haven’t been hospitalized since day one. I’d rather be chubby and alive than thin and in the psych ward. 🤷♀️
It’s wild how we treat bipolar like it’s a bug to be eradicated instead of a part of the human spectrum. The meds don’t fix you-they just give you space to be you without drowning in it. Maybe that’s the real goal: not to be ‘normal,’ but to be present.
Hey, if you’re struggling with side effects, you’re not alone. I started on lamotrigine and couldn’t sleep for weeks-felt like my brain was on fire. But after 3 months, it clicked. I’m sleeping, working, even dating again. It’s not perfect, but it’s mine. Keep going. You got this 💪
I tried quetiapine for a year. Slept 12 hours a day. Didn’t care if I missed work or forgot my kid’s birthday. I felt like a ghost in my own body. I switched to lurasidone-no weight gain, no brain fog. Took 6 weeks to adjust, but now I can laugh again. Not everyone’s experience is the same. Don’t give up on finding your fit.
Metformin saved my life. I was gaining 2 lbs a week on olanzapine. My doctor was hesitant, but I asked for it. Now I’ve lost 30 lbs, my blood sugar’s normal, and I don’t feel like I’m being slowly poisoned. If your doctor says ‘it’s just side effects,’ push back. You’re not exaggerating-you’re surviving.
Why do people keep saying ‘just take your meds’ like it’s a choice? I lost my job because I was too tired to get out of bed. I lost friends because I couldn’t be the person they wanted. And now I’m told I’m ‘non-compliant’? Fuck that. My brain isn’t broken-it’s been poisoned by pills that made me worse.
Regarding blood tests: even if you feel fine, lithium toxicity can silently damage your kidneys. I had a friend who skipped tests for six months. By the time he felt symptoms, his creatinine was 3.2. He needed dialysis for six weeks. Don’t gamble with your long-term health. Regular labs aren’t optional-they’re your lifeline.
I stopped lithium because I gained 40 pounds and my hair fell out. My doctor said, ‘It’s the price of stability.’ But I didn’t feel stable-I felt like a zombie with a side of shame. Then I found cariprazine. Minimal weight gain. No brain fog. I’m back at work. I’m back with my daughter. You don’t have to suffer to be well. Fight for the right med. You deserve more than survival-you deserve to live.