When you’re 75 or older, taking a simple pill can become risky-not because the medicine is dangerous, but because your kidneys don’t work the way they used to. About 30% of common medications for seniors are cleared from the body by the kidneys. If those kidneys aren’t working well, the drug builds up. That’s how you get dizziness, confusion, falls, or worse-kidney damage from something meant to help you.
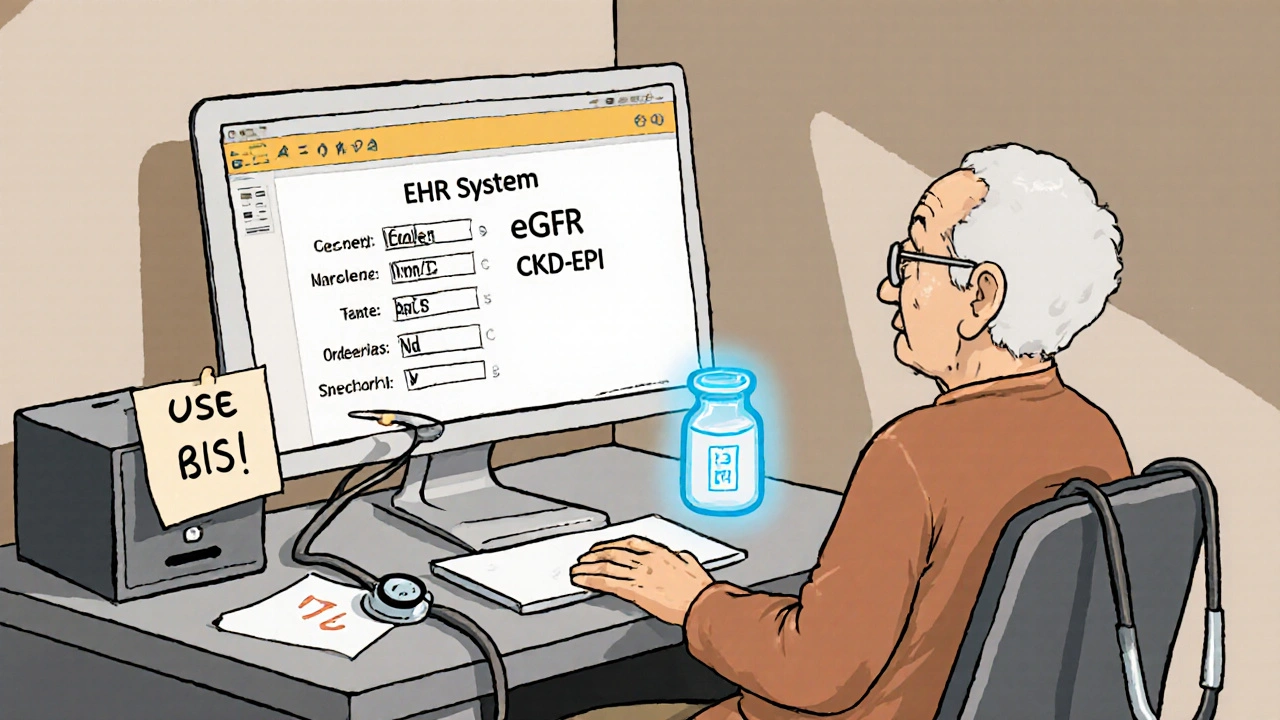
The problem isn’t that doctors don’t care. It’s that most of them are using the wrong tools to check kidney function. Many still rely on outdated formulas or let their electronic health records pick for them. And that’s where things go wrong.
Why Kidney Function Changes with Age
Your kidneys don’t suddenly stop working as you get older. But they do slow down. By age 70, the average person loses about 40% of their kidney filtering capacity compared to when they were 30. That’s normal aging-not disease. The tiny filters inside your kidneys, called nephrons, shrink and die off. Blood flow to the kidneys drops. Muscle mass decreases, which affects creatinine levels-the main marker doctors use to estimate kidney function.
This matters because most drugs are designed for healthy 30-year-old kidneys. If you’re 80 and your kidneys are filtering at 60% of their original speed, and you take the same dose as a younger person, you’re essentially overdosing. Medications like warfarin, digoxin, gabapentin, and even common painkillers like ibuprofen can build up to toxic levels. A 2024 study in Frontiers in Medicine found that using the wrong kidney function estimate led to 25% more dosing errors in seniors taking blood thinners like dabigatran.
The Four Equations That Actually Matter
There are four main ways to estimate kidney function. Only two are reliable for seniors-and even those have limits.
- Cockcroft-Gault (CG): This is the oldest formula, created in 1976. It uses age, weight, gender, and serum creatinine. The catch? It works best if you use ideal body weight, not your actual weight. For frail seniors or those with low muscle mass, using real weight overestimates kidney function by up to 30%. For obese seniors, it underestimates it. Studies show CG with ideal body weight reduces dosing errors by 25% compared to standard CG.
- MDRD: Introduced in 1999, this formula was meant to be more accurate than CG. But it was developed using younger adults. In seniors over 65, it tends to underestimate kidney function by about 1.4 mL/min/1.73 m². That might sound small, but it can push someone into a higher kidney disease stage than they’re actually in-leading to unnecessary dose reductions.
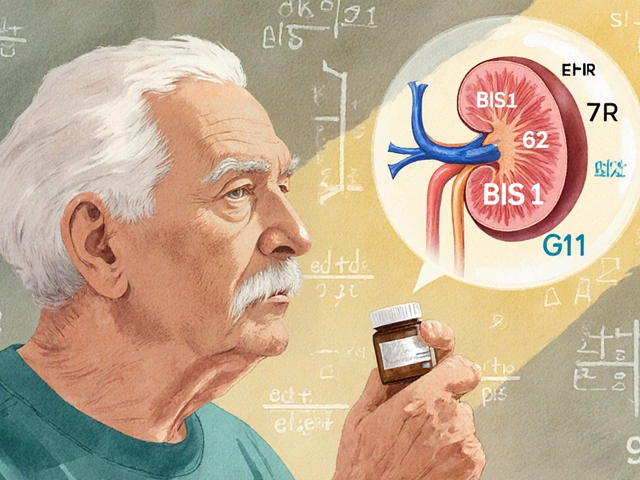
- CKD-EPI: This became the standard in 2009. It’s better than MDRD for most people, especially those with eGFR between 60 and 89. But for seniors over 75, especially those who are thin or malnourished, CKD-EPI still misclassifies kidney function in up to 30% of cases. A 2019 study found it often labels someone as Stage G2 when they’re really G3, which means they get less cautious dosing than they need.
- BIS1 and FAS: These are the new kids on the block. Developed specifically for older adults, they account for age-related muscle loss and other changes. BIS1, for example, correctly estimated kidney function in 95% of patients over 85, compared to just 78% for CKD-EPI. Dr. Sophie Dupont’s team at the University of Michigan found switching from CKD-EPI to BIS1 cut medication-related adverse events by 18% in patients over 80.
Here’s the truth: CKD-EPI is not the best for seniors. It’s the default because it’s built into most hospital systems. But it’s not designed for people who’ve lost muscle, eat poorly, or have chronic illness.
When to Use Cystatin C
There’s another test that doesn’t get used enough: serum cystatin C. Unlike creatinine, it’s not affected by muscle mass. It’s a cleaner signal of kidney function. The problem? It costs $50-$75 more than a basic creatinine test. Many clinics skip it because of cost.
But here’s when it’s worth it: if your creatinine-based eGFR is between 45 and 59 mL/min/1.73 m², but you have no diabetes, no high blood pressure, and no protein in your urine, your kidneys might actually be fine. Your low creatinine could just mean you have low muscle mass-not kidney disease. A cystatin C test can clear that up. If cystatin C says your kidneys are working normally, you might not need to cut your medication dose at all.
Dr. Maria Flamant, lead author of a major 2013 study, said it plainly: “CG with ideal body weight performed better than CKD-EPI in geriatric populations.” That’s still true today.
Real-World Mistakes and How to Avoid Them
Here’s what happens in real clinics:
- A 78-year-old woman with osteoporosis and low appetite has a creatinine of 1.1 mg/dL. Her EHR auto-calculates her eGFR as 58 using CKD-EPI. She’s told to cut her gabapentin dose. But her muscle mass is low. Her BIS1 eGFR is actually 72. She doesn’t need the dose cut-and cutting it leaves her in pain.
- A 92-year-old man with dementia and cachexia is on vancomycin. His creatinine is 1.3. CKD-EPI says his eGFR is 42. He gets a reduced dose. But his BIS1 eGFR is 28. He still gets too much drug and develops kidney injury.
These aren’t rare. A 2023 survey found 78% of pharmacists working with seniors have to override their EHR’s automatic kidney function calculation at least once a week. Why? Because the system doesn’t know if the patient is frail, underweight, or has low muscle mass.
Fixing this starts with asking three questions before prescribing:
- Is the patient over 75?
- Do they have low muscle mass, poor appetite, or recent weight loss?
- Is the medication narrow-therapeutic-index (meaning small changes in dose cause big effects)?
If you answered yes to any of these, don’t trust the EHR’s default. Use BIS1 or FAS. If you can’t get cystatin C, use Cockcroft-Gault with ideal body weight.
What’s Changing in 2025
Things are finally improving. Epic Systems, one of the biggest EHR vendors, now automatically uses BIS1 for patients over 75. The National Institute on Aging has launched a $4.2 million project called SAGE to build better point-of-care kidney tests for seniors. And in 2024, a new equation called CKD2024 was introduced-it combines creatinine and cystatin C with age-specific math. Early results show 15% better accuracy in patients over 80.
The FDA now requires drug labels to include dosing recommendations based on multiple eGFR equations. That’s huge. It means drug makers can’t just assume one formula works for everyone.
But until every clinic has these tools built in, you need to be your own advocate. If you’re a senior-or caring for one-ask your doctor: “Which equation are you using to check my kidney function? Is it the one made for older adults?”
What You Can Do Today
You don’t need to be a doctor to help. Here’s your action plan:
- Ask for your serum creatinine and eGFR numbers at every checkup. Don’t just accept “your kidneys are fine.”
- If you’re over 75, ask if BIS1 or FAS was used. If not, ask why not.
- If you’re on a drug like warfarin, digoxin, or an antibiotic like vancomycin, ask if your dose was adjusted based on your actual kidney function-not the default EHR number.
- Ask if cystatin C testing is an option, especially if your creatinine is borderline and you’re thin or weak.
- Use the National Kidney Foundation’s online eGFR calculator (updated 2023). It lets you compare results from different formulas side by side.
Medication safety in seniors isn’t about doing more tests. It’s about doing the right test. And that means moving past the one-size-fits-all approach that’s been around for decades.
The goal isn’t just to avoid toxicity. It’s to keep seniors active, independent, and pain-free-without unnecessary restrictions on their meds. That starts with knowing what your kidneys are really doing.
What’s the best way to check kidney function in seniors?
For seniors over 75, especially those who are frail, underweight, or have low muscle mass, the BIS1 or FAS equations are more accurate than the commonly used CKD-EPI. If those aren’t available, use the Cockcroft-Gault formula with ideal body weight-not actual weight. Always confirm with a doctor if your eGFR is borderline (45-59 mL/min/1.73 m²) and you have no signs of kidney disease.
Why does my doctor keep using CKD-EPI if it’s not the best for seniors?
Most electronic health records automatically use CKD-EPI because it’s the official guideline for general adult populations. Many doctors don’t realize it’s less accurate for older adults with low muscle mass. It’s not that they’re wrong-they’re using what the system tells them. Asking for BIS1 or FAS can make a big difference.
Can I trust my creatinine level to tell me if my kidneys are okay?
Not always. Creatinine comes from muscle. If you’ve lost muscle due to aging, illness, or poor nutrition, your creatinine level can be falsely low-even if your kidneys are failing. That’s why cystatin C is a better marker in seniors. It’s not affected by muscle mass. If your creatinine says your kidneys are fine but you feel weak or are on high-risk meds, ask for a cystatin C test.
Which medications are most dangerous if kidney function is miscalculated?
Drugs with narrow therapeutic windows are the most dangerous. These include blood thinners like dabigatran and rivaroxaban, antibiotics like vancomycin and aminoglycosides, heart drugs like digoxin, seizure meds like phenytoin, and pain relievers like gabapentin. Even common NSAIDs like ibuprofen can cause acute kidney injury if dosed too high in someone with reduced kidney function.
Should I get my kidney function checked every year?
Yes-if you’re over 65 and taking any regular medications, you should have your kidney function checked at least once a year. If you have diabetes, high blood pressure, heart disease, or have had a recent hospital stay, check every 6 months. Don’t wait for symptoms. Kidney damage often has none until it’s advanced.


Comments
CKD-EPI is garbage for seniors and everyone knows it except the EHR vendors who made billions off this outdated crap
My grandma got her gabapentin dose cut because of a fake eGFR and now she can't walk without falling
Doctors don't care they just click auto-calculate and move on
It's not medical negligence it's systemic laziness
You know, I've been thinking about this for a while, and it's not just about the equations-it's about how we see aging itself
We treat older bodies like broken machines that need fixing, instead of different machines that need recalibrating
The fact that we still use 30-year-old norms for 80-year-olds is like measuring a mountain with a ruler meant for a pencil
And don't get me started on how cystatin C is treated like a luxury test when it's literally the only honest signal we have
It's not about cost-it's about values
Why do we accept that seniors get less precise care? Why is their health treated as secondary?
I've watched my mother go through this-prescriptions adjusted based on numbers that didn't reflect her reality
She’s 79, eats like a bird, has no muscle left, but her EHR says her kidneys are 'mildly impaired'
Meanwhile, her real function? Probably normal
And yet, she's on half-doses of everything, barely sleeping, constantly tired
It's not medicine-it's a slow, quiet erasure
We need to stop letting algorithms decide who gets to live well
It's not about being a doctor
It's about being human
For anyone over 75 with low muscle mass, always use Cockcroft-Gault with ideal body weight
And if you can get cystatin C, do it
Don't trust the EHR
I'm a pharmacist and I override those auto-calcs daily
The clinical implications of misestimating GFR in geriatric populations are profound
Pharmacokinetic alterations secondary to age-related nephron loss necessitate equation-specific recalibration
BIS1 and FAS demonstrate superior sensitivity in cachectic cohorts
CKD-EPI's reliance on creatinine introduces significant bias in low-muscle phenotypes
Adopting cystatin C as a first-line biomarker would reduce iatrogenic toxicity by an estimated 22%
Until EHR systems are interoperable with geriatric-specific algorithms, clinician vigilance remains non-negotiable
Oh my goodness, this is exactly what my mum went through last year
She was on warfarin, and they reduced her dose because her eGFR was 52
But she's 81, weighs 48kg, hasn't eaten properly since her hip surgery
Turns out her BIS1 was 74
They put her back on the right dose and she's been dancing again
I can't believe this is still happening in 2025
It's not just medical-it's moral
And thank you for mentioning Epic's update
Finally, someone's listening
Every senior I know has been through this
Doctors trust the computer, not the person
We need to change the system, not just the equation
And yes, ask for cystatin C
It's worth every penny
THIS. So. Much.
I cried reading this
My dad almost died from a gabapentin overdose because they used CKD-EPI
He's 83, thin as a rail, eats oatmeal for dinner
His creatinine was 1.0
BIS1 said his kidneys were fine
Now he's pain-free and walking again
PLEASE share this with your doctor
❤️
I've seen this happen too
Not often talked about
But it's real
And it's preventable
Just asking the right questions saves lives
The article presents a compelling case for the adoption of geriatric-specific glomerular filtration rate estimation equations in clinical practice
It is imperative that healthcare providers recognize the limitations of creatinine-based estimations in elderly populations with sarcopenia
Empirical evidence supports the superiority of BIS1 and FAS in this cohort
Furthermore, the integration of cystatin C as a confirmatory biomarker represents a significant advancement in precision medicine for older adults
Systemic reform in electronic health record algorithmic defaults is not merely advisable-it is ethically obligatory
Look, I'm a nephrologist and I've been screaming about this for 15 years
CKD-EPI is for healthy adults, not 80-year-olds with no muscle and 2 teeth left
And don't even get me started on how EHRs ignore ideal body weight in CG
It's not just wrong-it's criminal
And yes, cystatin C is expensive
But so is a 90-year-old in the ICU from a drug overdose that never should've happened
Stop letting computers make decisions for you
Read the paper
Use BIS1
And if your clinic won't let you, go somewhere that will
❤️
This is the kind of info that changes lives
My aunt is doing so much better now that they switched to BIS1
She's back to gardening
And honestly?
It's not just about meds
It's about dignity
Keep sharing this
I'm from India and we don't have access to BIS1 or cystatin C in most clinics
But we can still use Cockcroft-Gault with ideal weight
It's not perfect
But it's better than what we have
And we can ask
That's the first step
I used to think my mom's fatigue was just aging
Turns out it was a too-low gabapentin dose
She couldn't walk to the bathroom without help
After switching to BIS1? She walked to the mailbox yesterday
I'm not a doctor
But I learned enough to ask
And that saved her
so like... the computer is wrong again??
surprise surprise
my grandma's eGFR was 48
she weighs 90lbs and hasn't eaten meat since 2019
turns out she just has no muscle??
who knew
also why does this cost $75??
we pay more for coffee